The Use of Virtual Reality Rehabilitation for Individuals Post Stroke
Gabrielly Marques Moreira1, Elis Marina Romão de Lima2, Ingrid Thaíse Machado2, Ana Paula Cunha Loureiro3, Elisangela Ferretti Manffra1*
1Health Technology Graduate Program, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil
2Physical Therapy Undergraduate Program, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil
3Department of Physical Therapy, School of Life Sciences, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil
Abstract
Background: Stroke causes somatosensory and motor deficits that compromise the static and dynamic balance. The recovery of these skills is an essential goal in the rehabilitation process and physiotherapy treatments have employed video games (VG) for therapeutic purposes.
Objective: To investigate the effects of employing VG in static and dynamic balance of individuals after stroke.
Design: Quasi-experimental study.
Method: The sample consisted of 28 individuals with hemiparesis, divided into experimental (EG) and control groups (CG), with 14 participants in each. The EG underwent conventional physiotherapy and commercial video games training. The interventions were individualized, with duration of 30 minutes, twice a week, for 10 sessions. The CG received only conventional physiotherapy. The groups were evaluated before and immediately after completion of the study. Individuals were assessed with Berg Balance Scale, MiniBESTest, Postural Assessment Scale for Stroke, Functional Reach Test and 1-minute sit-to-stand test.
Results: Both groups increased their scores on the scales. However, this increase was significant only for the EG in the Berg Balance Scale (p = 0.001), MiniBESTest (p = 0.001) and Functional Reach Test (p = 0.041). Correlation analysis indicated that the increase in functional scales was related to progress in the Tightrope game.
Conclusion: These results suggest that VG can be a valuable tool for physiotherapy practice, bringing potential benefits to improve static and dynamic balance in stroke individuals.
Introduction
Stroke is the most common cause of disability in Western countries and an important cause of death especially in the elderly. The probability of stroke is increasing specially when associated with risk factors such as atherosclerosis, smoking, alcoholism, sedentary lifestyle and obesity1. The sequels after a stroke may lead to motor, sensory, perceptual, and/or cognitive deficits and these impairments might impact on the individual functionality2.
Hemiparesis is a common consequence of a stroke which limits the functional performance and might persist for years. Due to the motor and somatosensory deficits, hemiparetic individuals present compromised postural reactions which depend on the integrity of the visual, vestibular, somatosensory and neuromuscular systems as well as the central commands for postural control3 Thus, the body balance condition after stroke is directly impacted by deficits on the proprioceptive inputs, the control of the trunk and the muscle strength. Moreover, the tendency to remain in an asymmetrical posture during standing, bearing less weight on affected side, might compromise activities of daily living and limit function4.
After a stroke, the improvement of the balance is an important objective for physiotherapy, which has a series of treatment modalities such as conventional physiotherapy5, aquatic physiotherapy6, electro-stimulation therapy7, proprioceptive neuromuscular Facilitation8 and Bobath approach9. However, there is a growing need for more motivating treatments able to promote neurofunctional recovery and to improve treatment adherence10. In this way, the digital technologies might be an interesting resource to be associated with other therapeutic approaches.
In fact, it has been shown that the use of video games (VG) aids in the practice of specific tasks by providing visual and auditory feedback, by promoting adaptive learning11 and neural plasticity12, by improving balance13,14, mobility15, range of motion16 and gait performance17.
Due to the importance of balance control after a stroke, task-oriented video games that stimulate this skill have been investigated14,15. A systematic review and meta-analysis19 aimed at investigating the effectiveness of VG in comparison to the absence of intervention or to other exercise interventions reported significant mean differences in favor of adding VG. The outcome measures that appeared in the review were the Timed Up and Go test (TUG), functional measures like Berg Balance Scale (BBS) and the anteroposterior postural sway. It is noticeable that TUG was the only mobility measure employed in the reviewed studies. Other meta-analysis, presented by Iruthayarajah et al.20, addressed the effect of balance training with VG for chronic stroke patients. They reported that VG promoted improvement of balance, which was observed in terms of BBS and the TUG. Nonetheless, the meta-analyses also suggest that other studies are necessary to confirm their findings, particularly for the most used video game system. A third meta-analysis, by Li et al.21, reported significant balance improvements among individuals with stroke, in all phases of recovery, for individuals using VG in comparison to controls. Again, the outcome measures were the the BBS and the TUG.
These studies have somewhat conflicting results and were mainly limited to few outcome measures, suggesting the need of further studies. Due to the great variety of scales and tests that can be employed in professional practice, their choice of tests must be made carefully, in order to detect the progression of the volunteer over time22 considering the skills that targeted in the therapy.
In spite that of the potential benefits of video games as therapeutic tools, the commercial ones have not been originally developed for people with disabilities as the stroke patients. Thus, it is important that the therapist chose a video game with tasks corresponding to the motor skills that are intended to be trained. Moreover, the choice of the outcome measures to assess the effect of therapy is also critical. In the case of balance training for post-stroke hemiparetic patients, games with activities that demand weight transfer between the paretic and non-paretic lower limbs may be an interesting alternative18. In the present study, we have selected games that stimulate lateral weight shifting and multidirectional balance in standing posture.
Thus, this study aimed to verify the effects of a commercial VG in improving balance among individuals with chronic stroke in relation to the improvement of balance with the use of diverse functional scales.
Methods
Individuals with chronic stroke were recruited among patients of the stroke outpatient department of the PUCPR University Physiotherapy Clinic and of the Ana Carolina Moura Xavier Rehabilitation Hospital in the city of Curitiba, Brazil. They should satisfy the following inclusion criteria: age above 18 years old, unique episode of unilateral stroke at least 6 months prior to recruitment, residual hemiparetic deficits, enrolled in a physiotherapeutic treatment, able to walk with or without assistive devices, able to give informed consent to participate in the research. Participants were excluded from the sample if they had global or major receptive aphasia, cognitive deficits, other neurological or orthopedic disorders, Brunnstrom recovery stages 1, 2 or 3 and uncorrectable visual impairment. This study was approved by the ethics review board of the University (report 1.360.987/2015). All participants provided written consent prior to data collection.
The study used convenience sampling recruited from a list of stroke patients provided by the therapists of the involved institutions. The volunteers were allocated in two groups: experimental (EG) and control (CG), with 14 subjects in each. The characteristics of the sample are set out in Table 1.
Patients were evaluated before and immediately after treatment. Initially, the patients underwent a physical examination and an interview for gathering clinical and demographical data, which included age, gender, body mass, height, time since stroke onset, associated diseases, strength (manual muscle test) and epicritic and protopathic sensitivity tests in the distal region of the lower limbs.
We have chosen five scales that evaluate different characteristics of balance: the Berg Balance Scale (BBS)23; MiniBESTest24; the Postural Assessment Scale for Stroke (PASS)25; the Functional Reach Test (FRT)26 and the 1 minute stand-sit test (1-MSTST)27. All selected tests and scales are valid and reliable in the stroke population. This variety of scales were employed because each outcome measure can serve to a specific purpose and has distinctive features and limitations. Therefore, we consider reasonable to apply different scales to cover different domains.
The Berg Balance Scale is a 14-item scale widely used for assessing balance. The items are scored from 0 (unable to execute the task) to 4 (independent) on the basis of the ability to complete a task, with the higher score indicating the degree of independence displayed while performing the tasks, for a maximum score of 5623.
The Mini-BESTest is a 14-item balance scale that measures dynamic balance, specifically anticipatory transitions, postural responses, and sensory orientation while standing on a compliant or inclined base of support, and dynamic stability during gait. Each task is rated on a 2-point ordinal scale from 0 to 2; a score of 0 indicates that a person is unable to perform the task; a score of 2 indicates normal performance. The maximum score for this scale is 2824.
The PASS is a postural assessment scale specifically designed to assess and monitor postural control after stroke. It contains 12 four-level items of varying difficulty for assessing ability to maintain or change a given lying, sitting, or standing posture. Each PASS item is rated on a scale from 0 to 3, for a maximum total score of 36: on this scale, the higher the score is, the more favorable the balance in stroke patients25.
The FRT is a scale used to measure the postural instability of an individual in the bipedal posture. With a tape measure parallel to the floor, the patient should lean forward with the nonparetic upper limb extended26.
The purpose of the 1-MSTST is to assess exercise capacity, leg muscle strength and to evaluate mobility. The patient sat with the knees and hips flexed to 90°, feet placed flat on the floor hip-width apart, and the hands placed on the hips. The movement required is to get up from the chair with the legs straight and sit back, continuing the repetitions as fast as possible within one minute. The number of repetitions was measured using a chronometer27.
All patients in this study attended a conventional physiotherapy program consisting of stretching exercises of the lower and upper limbs muscles, trunk control in sitting posture, coordination of upper limbs with sticks and march with parallel bars, which represents an average of 30 minutes a day of physical therapy twice a week. Participants of both control and experimental groups maintained their regular physiotherapy routine. Participants of the experimental were submitted to an additional balance training consisting of 30 minutes of therapy with the selected videogames, which dynamically stimulated bilateral anteroposterior and lateral medial weight transfer. The experiment lasted five weeks, covering ten intervention sessions.
For the intervention with the video game (VG), we have used the commercially available equipment Nintendo® Wii Fit Plus. It consists of a console coupled to a pressure-sensitive platform, the Wii Balance Board, and a remote control that allows selection among games that come with the equipment.
Three games were selected for this study which differed in the level of difficulty. All games aimed at improving postural control by increasing anteroposterior and mediolateral weight transfer in order to enhance the limits of stability of hemiparetic participants. The first game was Tightrope, it simulated the walking on a tightrope while the volunteer performed lateral-lateral displacement movements on the base of support. The second game was Balance Bubble which simulated the navigation in a bubble through a river while the volunteer made movements in the anteroposterior and mediolateral directions. In the third game - Penguin Slide - the participant had to catch fish while balancing on a floating ice cube; it is a demanding game, requiring rapid movements.
Before the intervention with the VG, the participants of the EG played every game without worrying about the correctness or about their performance. This was intended to create familiarity with the games and to help the volunteers to learn and to understand how to interact with the Balance Board. In the first six sessions the games Tightrope and Balance Bubble were applied. After that, the game Tightrope was replaced by the game Penguin Slide. Game score values were recorded at each repetition.
In the Tightrope and Balance Bubble the scores are measured in yards (yd), and the maximum possible scores are 40 yd and score of 1320 yd, respectively. In the Penguin Slide, there are fish of three different colors with different scores assigned to them. The maximal score in this game equals 136, when all red, blue and green fish have been captured.
At VG therapy, patients were instructed to stand on the Balance Board platform, which was 2 meters from a TV connected to the VG console. As a safety precaution, the Balance Board was surrounded by non-slip mats, reducing the risk of falling.
Data Analysis
Statistical analysis was performed using SPSS® software version 22.0 (IBM). Initially, the functional scale and game scores were tested for normality using the Shapiro-Wilk test. Since they are not normal data, non-parametric tests were applied to the rest of the analysis. To compare the scores of the groups, the Mann-Whitney test was applied. To compare the evaluation measures pre and post intervention, the Wilcoxon test was applied. The relationship between game and scale scores was established by Spearman correlation, indicated for non-normal data. The significance level was set at 0.05. The correction of Bonferroni applied to the Wilcoxon and Mann-Whitney tests: considering that four comparisons were done the corrected significance level was 0.0125.
References
The demographic and clinical features of the patients are summarized in Table 1. No significant differences between the general characteristics of the two groups were detected at recruitment. Significant differences between the groups were shown in balance after completing the exercise program. The intragroup analysis revealed that scores of BBS, MiniBESTest and FRT scales improved significantly for EG while the CG presented results close to those obtained in the initial evaluation of these scales (see Fig. 1 and Fig. 2). Both groups showed significant improvement measured by PASS and 1-MSTST. The mean values for the outcome measures at admission, and after 5 weeks for both groups are summarized in Table 2.
Table 1. Characteristics of the groups
|
Variables |
Control Group |
Experimental Group |
|
|
Gender – Women (%) |
50 |
42 |
|
|
Age (years) |
59 ( ± 10) |
52 ( ± 16) |
|
|
Body Mass (kg) |
73.5 ( ± 11) |
79.0 ( ± 17) |
|
|
Stature (cm) |
1.67 ( ± 10) |
1.68 ( ± 10) |
|
|
BMI (kg/m²) |
26.4 ( ± 10) |
28.0 ( ± 10) |
|
|
Stroke Etiology – Ischemic (%) |
57 |
57 |
|
|
Post-stroke time (months) |
16 ( ± 20) |
21 ( ± 17) |
|
|
Hemiparesis right (%) |
78 |
64 |
|
|
Dominance right (%) |
100 |
93 |
|
Values presented by mean and standard deviation.
BMI: Body Mass Index.
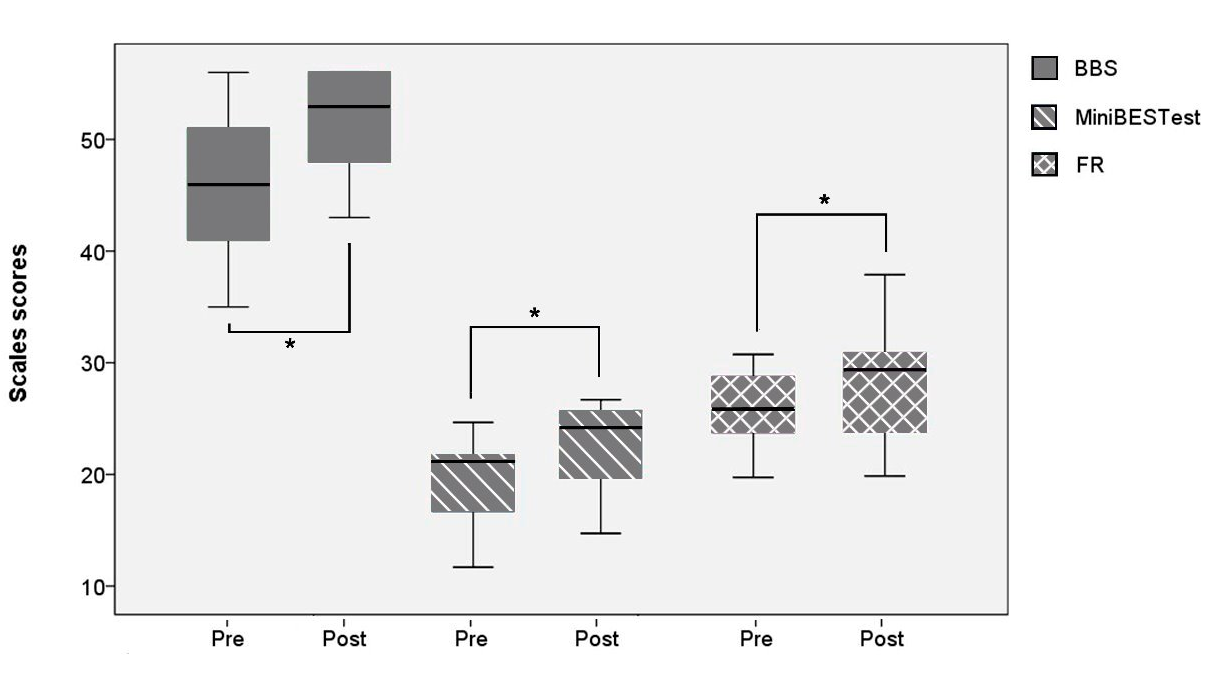
Figure 1: Functional scales of the experimental group (EG).
* Statistical significance in the Wilcoxon test.
Table 2. Scores of the functional scales of both groups
|
Groups |
BBS |
PASS |
MiniBESTest |
1- MSTST |
FRT |
|||||||
|
pre |
post |
pre |
post |
pre |
post |
pre |
post |
pre |
post |
|
||
|
Experimental Group |
Med |
46 |
53 |
29 |
33 |
20 |
24 |
15 |
18 |
26 |
29 |
|
|
Min |
35 |
43 |
17 |
26 |
11 |
15 |
4 |
6 |
16 |
20 |
|
|
|
Max |
56 |
56 |
35 |
36 |
24 |
27 |
26 |
30 |
31 |
38 |
|
|
|
IQR 1 |
40 |
47 |
25 |
29 |
25 |
19 |
10 |
12 |
23 |
23 |
|
|
|
IQR 3 |
51 |
56 |
34 |
34 |
34 |
26 |
17 |
21 |
29 |
31 |
|
|
|
W p-value |
0.001* |
0.005* |
0.001* |
0.011* |
0.041 |
|
||||||
|
Control |
Med |
40 |
45 |
23 |
29 |
18 |
18 |
10 |
14 |
24 |
25 |
|
|
Min |
30 |
15 |
14 |
19 |
12 |
10 |
4 |
5 |
20 |
15 |
|
|
|
Max |
56 |
56 |
36 |
36 |
22 |
23 |
24 |
30 |
30 |
25 |
|
|
|
IQR 1 |
32 |
34 |
17 |
22 |
13 |
14 |
6 |
7 |
20 |
22 |
|
|
|
IQR 3 |
48 |
50 |
31 |
32 |
21 |
20 |
16 |
17 |
26 |
25 |
|
|
|
W p-value |
0.609 |
0.005* |
0.888 |
0.004* |
0.505 |
|
||||||
|
M p-value |
0.080 |
0.011* |
0.097 |
0.042 |
0.287 |
0.004* |
0.166 |
0.249 |
0.158 |
0.031 |
|
|
*Statistical significance. Interquartile range 25% (IQR 1) and 75% (IQR3). W p-value: p-value of Wilcoxon test. M p-value: p-value of Mann-Whitney test.
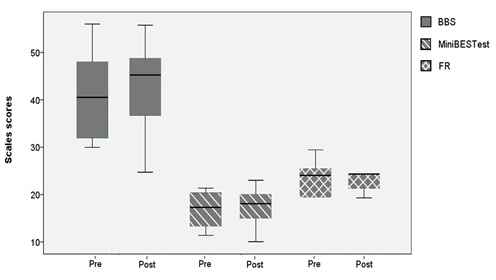
Figure 2: Functional scales of the control group (CG)
Regarding the VG applied to EG, it was possible to verify the existence of a positive and direct correlation between the scores of the game 1 - Tightrope and the BBS, MiniBESTest and PASS (Fig. 3). Different from the games 2 - Balance Bubble and 3 - Penguim Slide, which does not have connection with the scales (Figure 3). The p values and the correlation coefficients are shown in Table (3).
Table 3. Correlation between game and scale scores
|
Scales |
Game 1 |
Game 2 |
Game 3 |
|||
|
cf |
p - value |
cf |
p -value |
cf |
p -value |
|
|
BBS |
0.863 |
0.000* |
- 0.54 |
0.856 |
0.293 |
0.310 |
|
MiniBESTest |
0.701 |
0.005* |
0.016 |
0.958 |
- 0.222 |
0.446 |
|
PASS |
0.774 |
0.001* |
- 0.09 |
0.746 |
0.374 |
0.188 |
* Statistical significance. Correlation coefficient: cf
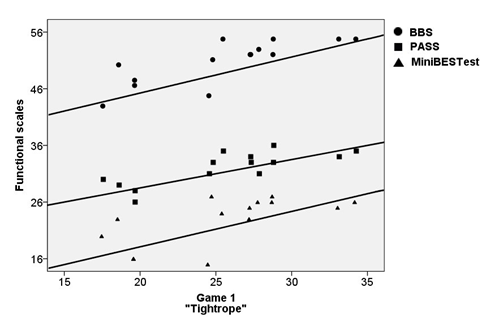
Figure 3: Correlation between the scores of the tightrope game and the functional scales
Discussion
The aim of the present study was to compare the effects of a commercial video game training in balance rehabilitation as an adjunctive therapy to conventional training in patients with chronic sequel from a stroke. Statistically significant improvements were found in the experimental group for all measures except in the 1-MSTST and the comparison with the control group revealed the VG assisted training was superior for increasing balance control according to the BBS, MiniBESTest.
Although both groups improved the results of the functional scales, only the virtual rehabilitation group showed a significant increase in the BBS and MiniBESTest scales, indicating that the VG might have an effect in increasing balance ability in chronic stroke individuals.
Cho; Lee; Song12 likewise reported improvement in dynamic balance of chronic stroke patients measured by BBS and TUG when compared to the control group after training with VG 3 times weekly for 6 weeks. The present study found similar results applying a shorter training protocol of 5 weeks intervention and show that balance gain persists during the chronic phase of stroke.
Morone et al.28, investigated the effect of VG intervention on balance of patients after stroke in the subacute phase. As in the present study, an improvement was observed in balance after four weeks of training in BBS score only in the VG group. The study showed that video game-based therapy also brings therapeutic benefits in the earliest phase post-stroke.
In this sense, also corroborating our findings, Utkan Karasu et al.29, described results after a rehabilitation balance program using VG in stroke chronic patients for a 4-week period, for 5 days a week and 20 min/d. They detected significantly greater improvements in the BBS and FRT compared with traditional treatment. However, the PASS values of the study reported no statistically significant differences between them, what differs from the current study. However, we have to take into account that PASS scale is more suitable for people with time 90 days after stroke.
Barcala et al.14 pointed out that 30 min/d of balance training using VG for five weeks, with two sessions per week plus conventional physical therapy sessions lasted 60 minutes, were not more beneficial than conventional therapeutic approaches to improve static balance assessed with stabilometric exam and dynamic balance as determined by the BBS and TUG. On the contrary, our study showed significant results in favor to experimental group in BBS and Mini-BESTest applying the same training protocol and same amount of exercise for both groups.
A study carried out by Hung et al.30 meanwhile using a longer intervention protocol, over 12 wk, 30 min/d, 2×/wk , compared the effects of VG with conventional weight-shift training on balance in individuals with chronic stroke , reported improvement in both groups in the TUG and FRT with no significant difference between them. The results of mentioned study are not consistent with our results which shows improvement in FRT in the experimental group. This difference could be due to the fact that our control group did not perform activities specifically directed to weight-shift training as the control group of the mentioned study.
Also contradictory to the present results, interventions using VG and progressive balance training in chronic stroke patients, 1 hour /d, 3x/ wk for 4 weeks, was reported by Yatar31. There were no difference between the two treatments in dynamic balance in BBS, TUG and FRT. However it was reported 8 weeks follow up that there was a decline in the BBS and TUG results in the group that didn't play VG.
The present study corroborates by another study Bower et al.32 that demonstrated results favour in the experimental group in balance measurement FRT, after 45 min/d, 3x/wk, over two to four weeks VG training in subjects in the early stages of stroke.
Singh et al.33 evaluated whether there were changes in the physical function when part of the standard physical therapy treatment was replaced by VG. Both groups improved their physical function (TUG and 30-second sitting and getting up test), however, no significant differences between groups were founded. Our results also showed significant improvement in 1-minute sit-to-stand test in both groups, but since the experimental group received 30 minutes of balance exercise using VG, in addition to 60 minutes of standard therapy, this greater volume of training might have affected our results.
Despite the significant improvements observed in terms of BBS, Mini-BESTest and PASS the change in STS test scores was not significant between groups. This could be justified by the fact that sitting and standing tasks and leg muscle strength comprising in the STS test not being addressed by the exercises performed with the VG.
In this study, the selected game 1 Tightrope seems to have been effective in training lateral weight shifting, which represents one of the first goals of physiotherapy treatment in order to improve postural control skills5, detected by the BBS, MiniBESTest and PASS.
Although our study found positive effects with respect to our outcomes, there are some limitations that must be addressed. One of the limitations of our study was that the CG did not receive the same amount of training than EG. Another limitation was that our sample was not randomly assigned into groups and examiners were not blinded. Also as a limitation was our short exercise program period, and no patient follows up to determine whether the benefits of the intervention are maintained over time.
Conclusion
Patients who completed the training using video games showed significantly greater improvement in their balance than those who only received traditional rehabilitation therapy. The results of this study indicate that video game exercise training combined with conventional training is a valuable tool for physiotherapy practice, bringing a positive impact on balance performance for patients with chronic stroke.
Acknowledgment
The authors thank the volunteers who agreed to participate in this study.
References
- Terranova TT. Chronic cerebral vascular accident: rehabilitation. Acta Fisiátrica. 2012; 19(2): pp. 50–59.
- Tyson S. Balance Disability after Stroke. Physical Therapy. 2006; 86 (1): 30-38.
- O'sullivan SB, SCHMITZ TJ. Fisioterapia: avaliação e tratamento. São Paulo: Manole. 2010.
- Genthon N, Rougier P, Gissot AS, et al. Contribution of each lower limb to upright standing in stroke patients. Stroke. 2008; 39 (1): pp. 1793–1799.
- Thompson PD1, Arena R, Riebe D, et al. ACSM’S new preparticipation health screening recommendations from ACSM’S guidelines for exercise testing and prescription. American College of Sports Medicine. 2013; 12 (4): pp. 215–217.
- Montagna JC, Santos BC, Battistuzzo CR, et al. Effects of aquatic physiotherapy on the improvement of balance and corporal symmetry in stroke survivors. Int J Clin Exp Med. 2014; 15 (4): 1182-7.
- Jonsdottir J, Thorsen R, Aprile I, et al. Arm rehabilitation in post stroke subjects: A randomized controlled trial on the efficacy of myoelectrically driven FES applied in a task-oriented approach. PLoS One. 2017; 4 (12): 10-13.
- Hwangbo PN, Kim D. Effects of proprioceptive neuromuscular facilitation neck pattern exercise on the ability to control the trunk and maintain balance in chronic stroke patients. J Phys Ther Sci. 2016; 28(3): 850-3.
- Benito García M, Atín Arratibel MÁ, Terradillos Azpiroz ME. The Bobath Concept in Walking Activity in Chronic Stroke Measured Through the International Classification of Functioning, Disability and Health. Physiother Res Int. 2015; 20(4): 242-50.
- Shin JH, Ryu H, Jang SH. A task-specific interactive game-based virtual reality rehabilitation system for patients with stroke: a usability test and two clinical experiments. J Neuroeng Rehabil. 2014; 11(2): pp. 11-32.
- Singh DK, Mohd Nordin NA, Abd Aziz NA, et al. Effects of substituting a portion of standard physiotherapy time with virtual reality games among community-dwelling stroke survivors. BMC Neurol. 2013; 13 (1): 199- 230.
- Cho KH, Lee KJ, Song CH. Virtual-Reality Balance Training with a Video-Game System Improves Dynamic Balance in Chronic Stroke Patients. Tohoku J Exp Med. 2012; 228 (1): 69-74.
- Orihuela-Espina F, Fernández del Castillo I, Palafox L, et al. Neural Reorganization Accompanying Upper Limb Motor Rehabilitation from Stroke with Virtual Reality-Based Gesture Therapy. Top Stroke Rehabil. 2013; 20 (3): 197–209.
- Barcala L, Grecco LA, Colella F, et al. Visual biofeedback balance training using wii fit after stroke: a randomized controlled trial. J Phys Ther Sci. 2013; 25 (8): 1027-32.
- Rajaratnam BS, Gui Kaien J, Lee Jialin K, et al. Does the Inclusion of Virtual Reality Games within Conventional Rehabilitation Enhance Balance Retraining after a Recent Episode of Stroke? Rehabilitation Research and Pract. 2013; 64 (1): 10-16.
- Mouawad MR, Doust CG, Max MD, et al. Wii-based movement therapy to promote improved upper extremity function post-stroke: A pilot study. J Rehabil Med. 2011; 43(6): 527-33.
- Walker ML, Ringleb SI, Maihafer GC, et al. Virtual Reality-Enhanced Partial Body Weight-Supported Treadmill Training Poststroke: Feasibility and Effectiveness in 6 Subjects. Arch Phys Med Rehabil. 2010; 91(1): 115–22.
- Turolla A, Dam M, Ventura L, et al. Virtual reality for the rehabilitation of the upper limb motor function after stroke: a prospective controlled trial. J Neuroeng Rehabil. 2013; 10 (1): 85.
- Cheok G, Tan D, Low A, et al. Is Nintendo Wii an Effective Intervention for Individuals With Stroke? A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2015; 16(11): 923-32.
- Iruthayarajah J, McIntyre A, Cotoi A, et al. The use of virtual reality for balance among individuals with chronic stroke: a systematic review and meta-analysis. Top Stroke Rehabil. 2017; 24(1): 68-79.
- Li Z, Han XG, Sheng J, et al. Virtual reality for improving balance in patients after stroke: A systematic review and meta-analysis. Clin Rehabil. 2016; 30(5): 432–440.
- Acosta AM, Dewald HA, Dewald JP. Pilot study to test effectiveness of video game on reaching performance in stroke. J Rehabil Res Dev. 2011; 48 (4): 431–444.
- Blum L, Bitensky NK. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008; 88 (5): 559-66.
- Potter K, Brandfass K. The Mini-Balance Evaluation Systems Test (Mini-BESTest). Journal of Physiotherapy. 2015; 61 (1): 225.
- Yoneyama S. Validation of the Brazilian version of the Postural Assessment Scale for Stroke Patients. Acta Fisiatr. 2008; 15 (2): 96–100.
- Acosta AM, Dewald HA, Dewald JP. Pilot study to test effectiveness of video game on reaching performance in stroke. J Rehabil Res Dev. 2011; 48 (4): 431–444.
- Bohannon RW, Crouch R. 1-Minute Sit-to-Stand Test: Systematic Review of Procedures, Performance, and Clinimetric Properties. J Cardiopulm Rehabil Prev. 2019; 39(1): 2-8.
- Morone G, Tramontano M, Iosa M, et al. The efficacy of balance training with video game-based therapy in subacute stroke patients: a randomized controlled trial. Biomed Research International. 2014; 580861(1): 1-6.
- Karasu AU, Batur EB, KarataÅ GK. Effectiveness of Wii-Based Rehabilitation in Stroke: A Randomized Controlled Study. J Rehabil Med. 2018; 50(1): 406–412.
- Hung JW, Chou CX, Hsieh YW, et al. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch Phys Med Rehabil. 2014; 95(9): 1629-37.
- Yatar GI, Yildirim SA. Wii Fit balance training or progressive balance training in patients with chronic stroke: a randomized controlled trial. J Phys Ther Sci. 2015; 27(4): 1145-51.
- Bower KJ, Clark RA, McGinley JL, et al. Clinical feasibility of the Nintendo Wii for balance training post-stroke: a phase II randomized controlled trial in an inpatient setting. Clin Rehabil. 2014; 28: 912–923.
- Singh DK, Mohd Nordin NA, Abd Aziz NA, et al. Effects of substituting a portion of standard physiotherapy time with virtual reality games among community-dwelling stroke survivors. BMC Neurol. 2013; 13 (1): 1319.
