Base for Physiotherapeutic Treatment Recommendations for Long COVID-19 Patients After Questioning Experienced Physiotherapists Using a Delphi Method
Chloé Schorderet1,2,3*, Roger Hilfiker4, Lara Allet1,2,5
1School of Health Sciences, HES-SO Valais-Wallis, University of Applied Sciences and Arts Western Switzerland, Valais, Sion, Switzerland
2The Sense Innovation & Research Center, Lausanne and Sion, Switzerland
3Department of Epidemiology, Care and Public Health Research Institute (CAPHRI), Maastricht University, Maastricht, Netherlands
4School of Health Sciences, HES-SO Valais-Wallis, University of Applied Sciences and Arts Western Switzerland, Valais, Leukerbad, Switzerland
5Department of Community Medicine, University Hospitals and University of Geneva, Geneva, Switzerland
Abstract
Background: Long COVID-19 is frequently observed in people who have contracted SARS-COV-2. It is characterized by a set of symptoms that can persist for months after infection and represents a challenge for all health care professionals. Among them, physiotherapists play an essential role thanks to their extensive knowledge in the rehabilitation field. To provide quality treatment, they need recommendations on which to rely. The aim of this study is to gather opinions from therapists working in Europe on the management of long COVID-19 patients in physiotherapy.
Method: A Delphi method was conducted in three rounds. In the first round, participants were asked about the deficits observed in long COVID-19 patients and about tests, monitoring and treatment to be implemented during the treatment of these patients. During the second and third rounds, they were informed about the results already obtained and had to confirm their answers with 6-point Likert scales.
Results: The most frequently observed impairments were pain, reduction in general physical fitness and respiratory problems. For assessment and treatment, the responses are specific to each impairment category. The 6-minute test seems to be particularly relevant for the assessment of several deficits and active approaches seem to have an essential place in the treatment.
Conclusion: Our study highlighted the diversity of impairments observed by physiotherapists in long COVID-19 patients and allowed to create a consensus on the assessments and treatments to be preferred for each type of impairment. In general, active treatment should be preferred for most of the impairments for which long COVID-19 patients consult a physiotherapist.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a highly contagious virus affecting the lower respiratory tract and causing pneumonia in humans1. It causes a variety of symptoms ranging from asymptomatic or mild symptoms to serious illness and death2. The most common symptoms are coughing, fever and shortness of breath2. In some cases, serious impairments, especially respiratory, are present3. The virus can also cause neurological, musculoskeletal, and cardiovascular impairments4.
Many authors reported that symptoms persist after the acute phase. Greenhalgh et al. indicated that about 10% of people who contracted the SARS-CoV-2 suffered from symptoms for more than three weeks5. This was also demonstrated by Sudre et al. who reported that 13.3% of patients had symptoms lasting more than 28 days6. Carfi et al. also investigated the symptom persistence after the acute phase7. They showed that about 87% of patients hospitalized because of the virus still experience at least one symptom nearly two months after hospitalization. The most common symptoms were fatigue, dyspnea, joint pain, and chest pain7. These symptom have a major impact on the quality of life of patients who were infected by COVID-198. Halpin et al. reported a significant reduction on the EQ5D score in 68.8% of participants who were in ICU and in 45.6% of participants who were hospitalized after an infection due to COVID-19 (between 29 and 71 post discharge)9.
Symptoms that persist or appear after the acute phase of a SARS-CoV-2 infection are defined by the term “long COVID”. The term long COVID includes symptoms lasting between 4 and 12 weeks after the acute phase and also the post-COVID syndrome that refers to symptoms lasting for 12 weeks or more8. Long COVID affects 145 million people worldwide10 and it was reported that a prolonged duration of rehabilitation can be expected for long COVID-19 patients, particularly for those who have been severely affected11. Symptoms suffered by patients with long COVID are very varied and the most persistent seem to be fatigue and shortness of breath12.
The diversity and persistence of illness associated with SARS-CoV-2 infection is a challenge for different health care professionals and the entire health care system. Among the professionals concerned, physiotherapists play a central role13 as they have a very advanced knowledge in the field of rehabilitation. Authors reported that a multidisciplinary rehabilitation is necessary which should be based on the observed deficits and focus on the musculoskeletal system and the functional rehabilitation14.
In this context, it is important that physiotherapists can rely on clear recommendations. Research on the rehabilitation of patients with COVID-19 is ongoing and various recommendations were already proposed14-18. However, to our knowledge, there are no studies that provide an overview of suggestions for physiotherapists' practices.
Aim
The aim of this study is to create a consensus on practice recommendations for physiotherapists in the management of long COVID-19 patients. This consensus aims to describe assessments and treatments (monitoring, volume, frequency, and content) to be recommended during the rehabilitation of long COVID-19 patients.
Method
Design
A Delphi method was used to create a consensus on practice recommendations for physiotherapists in the treatment of long COVID-19 patients.
Inclusion criteria for participant selection
To be eligible for the study, participants of the Delphi Round had to meet at least one of the following two criteria: (1) be a physiotherapist with experience treating long COVID-19 patients (at least 10 long COVID-19 patients treated) (2) be a physiotherapist and be the author of a publication related to physiotherapy in patients with SARS-CoV-2 / long COVID-19 patients. Thus, we could guarantee a group of participants with good practical and scientific knowledge who had sufficient legitimacy to express an opinion representing that of physiotherapists treating long COVID-19 patients.
Participant recruitment
We recruited participants by sending emails to the physiotherapy departments of large hospitals and rehabilitation centers in Switzerland and major European cities. The physiotherapy departments were informed of the aim of our study and were asked to provide us with the contacts of physiotherapists interested in participating. We also contacted by email physiotherapists, who were authors of publications related to COVID-19 and physiotherapy. We contacted a total of 119 physiotherapy departments/authors and 44 physiotherapists agreed to participate in the Delphi. Regarding sample size, authors reported that a group of 10 to 15 participants is sufficient if the group is sufficiently homogeneous19, which is the case in our study since all participants are physiotherapists treating or conducting research on patients suffering from COVID-19. However, we recruited more than 15 participants to ensure that we would have enough participants if some dropped out during the study.
Preparation phase
We used an explanatory sequential design20 to collect data to prepare the initial survey for the Delphi. Two members of the research team conducted semi-structured interviews with five physiotherapists regularly treating patients infected by SARS-CoV-2. These interviews were conducted online and lasted between 20 and 55 minutes. The questions focused on observed deficiencies due to COVID-19 infection. At the same time, we performed a literature search in PubMed and Google Scholar about symptoms due to COVID-19 infection.
Semi-structured interviews and results of literature search allowed us to identify the main impairments observed in long COVID-19 patients. We classified them into seven categories: (1) pain, (2) general physical fitness, (3) respiratory problems, (4) strength deficits, (5) joint mobility restrictions, (6) balance deficits, (7) other. Each category contained sub-categories of impairments which are presented in Table 1.
Table 1: Summary of categories and sub-categories of impairments in long COVID-19 patients.
|
1. PAIN |
|
· Generalized pain/widespread pain · Muscle pain · Nerve pain · Joint pain · Skin pain |
|
2. GENERAL PHYSICAL FITNESS |
|
· Reduced general physical fitness at the beginning of the rehabilitation · Reduced general physical fitness in the middle of the rehabilitation · Reduced general physical fitness at the end of the rehabilitation |
|
3. RESPIRATORY PROBLEMS |
|
· Dyspnea · Hypoxemia · Pulmonary obstruction · Hyperventilation · Pulmonary fibrosis · Strength deficits |
|
4. STRENGTH DEFICITS |
|
· Muscle mass deficit · Muscle power deficit · Muscle endurance deficit · Maximal strength deficit · Reduced rate of force development |
|
5. JOINT MOBILITY RESTRICTIONS |
|
6. BALANCE DEFICITS |
|
· Static balance deficit · Perturbed sensory orientation · Perturbed reactive postural adjustments · Reduced gait stability |
|
7. OTHER DISORDERS |
|
· Fatigue · Anxiety · Dysphagia · Stress · Dizziness · Troubles of intellectual functions · Disorientation · Attention problems · Feeling of stigmatization |
Establishment of the Delphi
We established the survey for the first Delphi round based on the reported impairments that we classified in seven categories. The survey was written in English, a language common to all participants and made available via the REDCap software (REDCap 8.5.11 - © 2020), which allowed to code the participants' names to ensure that the research team's analyses remained neutral. The survey is described in detail in chapter “Round 1”.
Before diffusing the online survey, it was sent for a pre-test to 5 physiotherapists treating patients suffering from long COVID-19 with the request to check and point out problems with orthography and grammar, to check the clarity of the questions, and to signalize any technical issues.
The research team made the necessary changes following these pre-tests and started then the data collection period which was between September 2020 to February 2021. Between each round, the data were analyzed and feedback were given to the participants presenting the results in an anonymous way19. Overall, three rounds were necessary to achieve a consensus.
Round 1
The questionnaire of the first round consisted of three parts. The first part contained general questions concerning participants (age, gender, professional background, work location, work domain, number of treated long COVID-19 patients). The second part included questions on the mean time after which long COVID-19 patients started physiotherapy after an ICU stay, the mean duration of physiotherapy treatment and the recommended frequency of physiotherapy sessions. The third part contained questions related to the impairments mentioned in Table 1. Participants were asked to rate how often they observed each impairment in long COVID-19 patients on a scale from 0 to 100 (0 corresponding to never and 100 corresponding to always). For pain, we asked questions related to intensity and location. For strength deficits, we asked to indicate the affected body area. Furthermore, participants were asked questions about the assessment and treatment of each impairment. They could make their own proposals or choose between responses proposed by the research team (based on the literature search and on semi-structured interviews).
Round 2
For the second round, we send to the participants (1) a summary of the first round describing the main impairments observed in long COVID-19 patients and their frequency and (2) the second survey. In the second survey, we took over all questions of the first survey concerning assessment and treatment of each type of impairment and we presented the answers of the participants as follows:
- For the open-ended questions from the first survey, we proposed all the answers cited by the participants.
- For the multiple-choice questions from the first survey, we selected only the answers chosen by more than 10% of the participants who answered the question. These answers were ranked from the most to the least chosen during the first round and this information was given to the participants in the question heading.
For each proposal, we asked the participants to rate their agreement on a 6-point Likert scale containing the following response options “strongly disagree”, “disagree”, “neutral”, “agree”, “strongly agree”, and “N. E.” (no experience, participants were invited to check this option if they did not feel experienced enough in the field to answer the question).
According to Minkman et al.21, at the end of the second round, the assessments, and treatments for which more than 80% of participants responded “agree” or “strongly agree” were directly retained in the consensus; the assessments and treatments for which between 50 and 79% of participants responded “agree” or “strongly agree” were retained for the third round; and the assessments and treatments for which less than 50% of participants responded “agree” or “strongly agree” were excluded.
Round 3
In the third-round participants were asked to judge again the assessments and treatment options for which 50 to 79.9% of the participants answered "agree" or "strongly agree" during the second round. They were informed about the rate of agreement obtained in the second round for each assessment, respectively treatment. Before each question, the participants were informed about the assessment and treatment options already retained in the consensus (proposals for which more than 80% of the participants answered "agree" or "strongly). In addition, the participants received a summary with the assessment and treatment options not retained in the consensus (proposals for which less than 50% of the participants responded "agree" or "strongly agree" in the previous round). At the end of the third round, the assessments, and treatments for which more than 70% of the participants answered “agree” or “strongly agree” were retained in the consensus.
Data analysis
We performed descriptive statistics with the Excel Software and with the RStudio software. We calculated the frequency with which physiotherapists reported that they encountered impairments and expressed it in percentage (the % of physiotherapists among all participating physiotherapists). In addition, the time between the ICU discharge and the start of an ambulatory/rehabilitation treatment, the duration of physiotherapy treatment, the recommended frequency of physiotherapy sessions and the number of long COVID-19 patients already treated were calculated and expressed in means and standard deviations (SD). As regards to suggested assessments and treatments, the rate of agreement between participants was calculated in percentages for each answer.
Results
34 people participated in the first round, which occurred between September 9 and September 30, 2020; 29 people participated in the second round which occurred between November 23 and December 17, 2020; and 24 people participated in the third round which occurred between January 28 and February 18, 2021. Characteristics of participants from the third round are presented in Table 2.
Table 2: Participant’s characteristics.
|
Gender |
Women: 50% Men: 50% |
|
Age |
35.71 years old (SD=9.98) |
|
Professional background |
Philosophiæ doctor (PhD): 12.5% Master of Science (MSc): 37.5% Bachelor of Science (BSc): 45.8% Other: 8.3% |
|
Work location |
Hospital: 87.5% Physiotherapy practice: 12.5% Research: 25% Rehabilitation: 8.3% |
|
Work domain |
Musculoskeletal: 12.5% Respiratory care: 75% Cardiology: 41.7% Neurology: 33.3% Other: 0% |
|
Country |
Switzerland: 62.5% Italy: 12.5% France: 8.3% Austria: 8.3% Spain: 4.2% Irland: 4.2% |
Based on the results of the first round, participants treated in average 36 long COVID-19 patients (mean (±SD): 36±60.59). This average rapidly increased and reached an average of 75 treated long COVID-19 patients per participant in the third round (mean (±SD): 75±93.47).
During the first round, participants reported that long COVID-19 patients came to physiotherapy on average 4.56 weeks after discharge of the intensive care (mean (±SD): 4.56±4.39). Results regarding the mean duration of physiotherapy treatment for long COVID-19 patients are presented in Figure 1. Results related to the recommended frequency of physiotherapy sessions for long COVID-19 patients are presented in Figure 2.
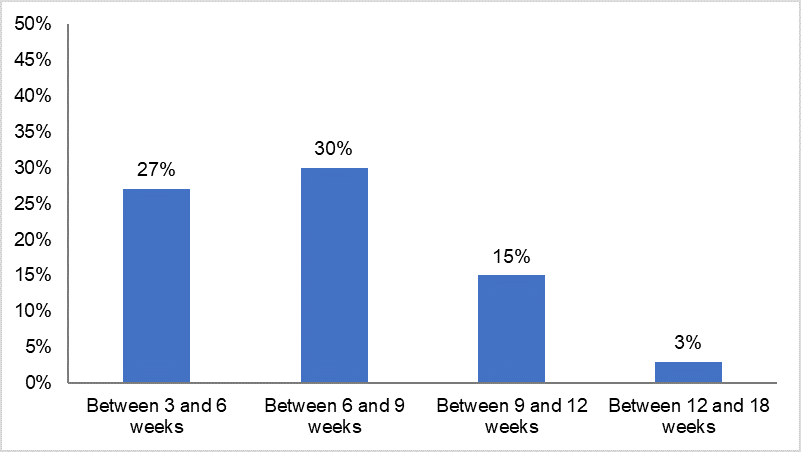
Figure 1: MEAN DURATION OF PHYSIOTHERAPY TREATMENT IN LONG COVID-19 PATIENTS. Percentage of physiotherapists per duration of physiotherapy treatment.
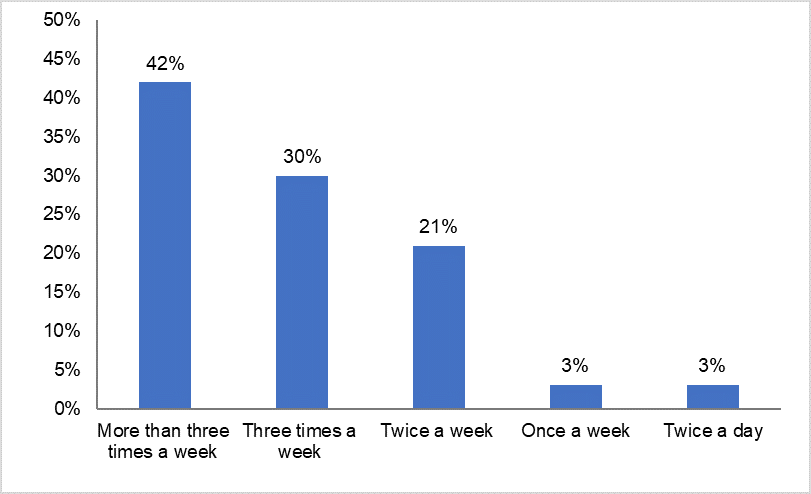
Figure 2: RECOMMENDED FREQUENCY OF PHYSIOTHERAPY SESSIONS FOR LONG COVID-19 PATIENTS. Percentage of physiotherapists per recommended frequency of physiotherapy sessions
Observed impairments
A summary of the impairments observed by physiotherapists in long COVID-19 patients is presented in Figure 3. The most frequently observed impairments were pain (observed by 94% of participants), reduction in general physical fitness (observed by 85% of participants) and respiratory problems (observed by 82% of participants). Regarding joint mobility restrictions, shoulders and ankles were the most affected joints.
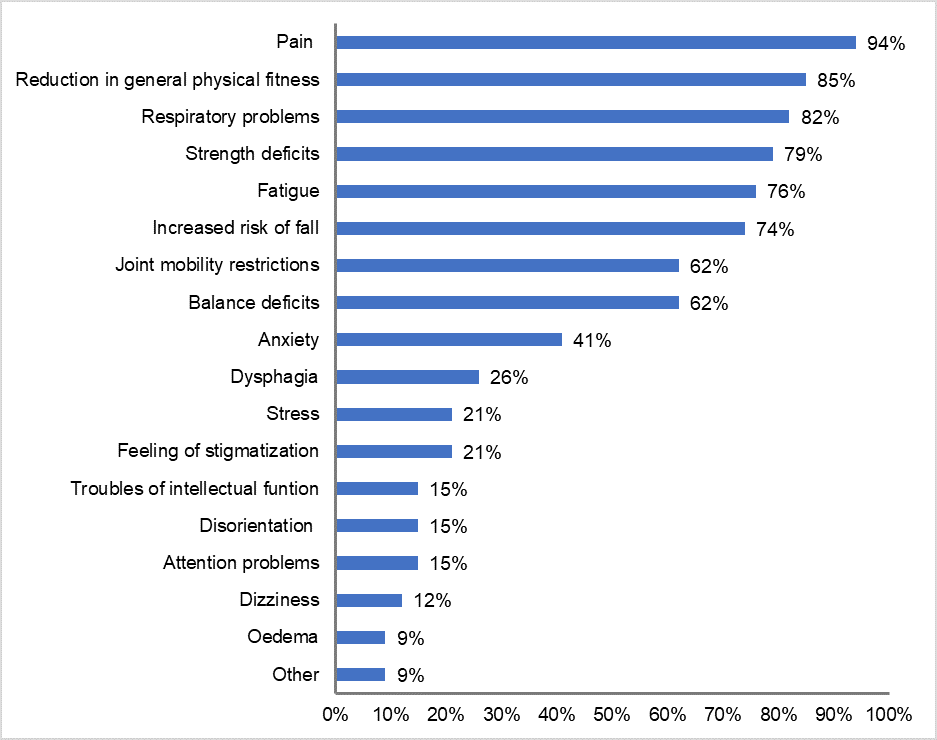
Figure 3: IMPAIRMENTS OBSERVED BY PHYSIOTHERAPISTS IN LONG COVID-19 PATIENTS. Percentage of physiotherapists observing the mentioned impairments in long COVID-19 patients.
Assessment and treatment of pain
Items that reached consensus for assessment and treatment of each type of pain are presented in Table 3. Regarding pain assessment, the use of the NRS and the use of the VAS were retained for all types of pain. In addition, asking for subjective feedback was retained for assessing muscle pain; a neurological physical examination was retained for assessing nerve pain; and the range of motion test was retained for assessing joint pain. Regarding pain treatment, participants agreed that active therapies such as graded activity, exercising, physical activity, and active mobilization should be used to treat all types of pain. In addition, counseling was retained for treating muscle pain, nerve pain and skin pain.
Table 3: Assessment and treatment of pain in long COVID-19 patients.
|
|
ASSESSMENT |
TREATMENT |
|
Generalized pain / widespread pain
|
• Numeric Rating Scale (NRS) (79%; 95%) • Visual Analog Scale (VAS) (74%; 90%)
|
• Graded activity (97%) • Gentle exercises (86%) • General mobilization (86%) • Pain medication (64%; 77%) |
|
Muscle pain
|
• Numeric rating scale (NRS) (83%) • Visual Analog Scale (VAS) (82%) • Asking for subjective feedback (74%; 90%) |
• Exercise/physical activity (100%) • Muscle endurance training (81%) • Continuous endurance training (77%; 100%) • Counseling (75%; 86%) |
|
Nerve pain
|
• Numeric rating scale (NRS) (85%) • Visual Analog Scale (VAS) (81%) • Neurological physical examination (80%) |
• Physical activity (100%) • Sensomotoric therapy (82%) • Neural-mobilization techniques (78%; 83%) • Counseling (67%; 84%) |
|
Joint pain
|
• Visual Analog Scale (VAS) (96%) • Numeric rating scale (NRS) (96%) • Range of motion (ROM) test (92%) |
• Active mobilization of the affected joint (96%) • Passive mobilization of the affected joint (83%) • Stretching (70%; 79%) |
|
Skin pain |
• Visual Analog Scale (VAS) (96%) • Numeric rating scale (NRS) (96%) |
• Physical activity (87%) • Frequent position changes (86%) • Graded activity (78%; 89%) • Counseling (76%; 74%) |
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
Assessment and treatment of reduced general physical fitness
The different assessments and treatment options that reached consensus for the management of reduced general physical fitness at the beginning, in the middle and at the end of the rehabilitation ("rehabilitation" mean here the period during which a patient is treated in physiotherapy) are presented in Table 4.1. Regarding the assessment of reduced general physical fitness, tests to be used depend on the patient's abilities. As standard assessment, the 6 Minute Walk Test, the 1-Minute Sit-to-Stand Test and the spiroergometric test were retained in the consensus. For patients who cannot walk but can stand, the 1-Minute Sit-to-Stand Test and the Hand Grip Strength Test were retained in the consensus; and for patients who cannot stand, the Hand Grip Strength Test was retained in the consensus.
Table 4.1: Assessment and treatment of general physical fitness in long COVID-19 patients.
|
ASSESSMENT |
||
|
Standard assessment: • 6 Minute Walk Test (93%) • 1-Minute Sit-to-Stand Test (77%; 95%) • Spiroergometric test (73%; 75%) Assessment if patient cannot walk enough to do a walking test but is able to stand: • 1-Minute Sit-to-Stand Test (80%) • Hand Grip Strength Test (76%; 78%) Assessment if patient is not able to stand: • Hand Grip Strength Test (84%) |
||
|
TREATMENT * |
||
|
At the beginning of the rehabilitation: • Muscle endurance training (96%) • Respiratory muscles training (84%) • Continuous endurance training (81%)
|
In the middle of the rehabilitation: • Muscle endurance training (100%) • Continuous endurance training (96%) • Respiratory muscle training (80%) • Hypertrophy training (72%; 79%) • Intermuscular/intramuscular coordination training (68%; 78%) |
At the end of the rehabilitation • Muscle endurance training (96%) • Continuous endurance training (96%) • High intensity interval training (89%) • Hypertrophy training (76%; 78%) • Respiratory muscle training (72%; 75%) |
|
VOLUME |
||
|
• Post-COVID-19 inpatients should train at least 30 minutes each day (85%) • Post-COVID-19 outpatients (should train at least 30 minutes 3 times/week (100%) |
||
|
PARAMETERS TO MONITOR |
||
|
• Oxygen saturation (100%) • Heart rate (100%) • Dyspnea (100%) • Clinical signs (e.g., trembling of muscles, paleness, sweeting) (95%) |
||
|
CONDITION UNDER WHICH PARAMETERS SHOULD BE MONITORED |
||
|
• At rest (95%) • Directly after exercise (95%) • During exercise (90%) • 2 minutes after exercise (85%)95%) |
||
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
* Supplementary information for each type of training is presented in Table 4.2.
Table 4.2: Training modalities
|
|
Assessment training intensity |
Recommended intensity |
Recommended volume |
|
High intensity interval training |
• Modified Borg scale (0-10) (96%) • % of max Watts (86%) • % of SPO2 (78%; 74%) • % of maximal heart rate (70%; 79%) • Borg scale (6-20) (57%; 78%) |
• FOR THE PERIOD OF HIGH INTENSITY: Moderate to vigorous intensity (defined as 60% of VO2 max; 74% of max Heart Rate; 60% of Heart Rate Reserve; Modified Borg 6; patient can speak but not sing a song) (88%) • FOR THE RECOVERY PERIOD: Low intensity (defined as 45% of VO2 max; Modified Borg 3; patient can speak but not entirely comfortably) for the recovery period during high intensity interval training (88%) |
• Periods of 1-minute of high intensity exercise followed by periods of 1-minute of recovery (90%) |
|
Muscle endurance training |
• Modified Borg scale (0-10) (100%) • % of max Watts (64%; 76%) |
• Moderate to vigorous intensity (defined as 50-65% of 1RM; modified Borg 5-6/10) (96%) |
• 2-3 sets of 15-20 repetitions (91%) |
|
Continuous endurance training |
• Modified Borg scale (0-10) (100%) • % of SP02 (78%; 78%) • % of max Watts (77%; 94%) • % of max heart rate (70%; 94%) • Borg 6 - 20 (50%; 71%) |
• Moderate to vigorous intensity (defined as 60% of VO2 max; 74% of max Heart Rate; 60% of Heart Rate Reserve; Modified Borg 6; patient can speak but not sing a song) (100%) • Low intensity (defined as 45-50% of VO2 max; 65% of max Heart Rate; 50% of Heart Rate Reserve; Modified Borg 3-4; patient breaths faster but can still speak using full sentences) (82%) |
• More than 30 minutes (70%; 83%) |
|
Hypertrophy training |
• % of one-repetition maximum (1RM) (94%) • Modified Borg scale 0-10 (90%) • Quality of movement (80%) |
• Level corresponding to 70-85% of 1RM; Borg 15/20; OMNI-RES 7-8; 8-12 possible repetitions (89%) |
• Volume of 3-4 sets of 8-12 repetitions (79%; 94%) |
|
Maximal strength training |
• Modified Borg Scale 0-10 (90%) • Clinical signs (e.g., muscle trembling) (85%) • % of one-repetition maximum (1RM) (80%) • Quality of movement (76%; 94%) • Subjective fatigue of the muscle (70%; 82%) |
|
• 3-6 sets of 1-6 repetitions (83%) |
|
High speed power training |
• Modified Borg scale 0-10 (82%) • Velocity during movement (64%; 75%) • OMNI-RES scale (57%; 33%) • Quality of movement (55%; 85%) |
|
|
|
Plyometric training |
|
|
• 3-5 sets of 6-12 repetitions (53%; 75%) |
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
Participants further agreed that muscle endurance training, continuous endurance training and respiratory muscle training should be performed during whole rehabilitation process to face reduced general physical fitness. In addition, consensus was reached for the use of hypertrophy training in the middle and at the end of the rehabilitation, for intermuscular and intramuscular training in the middle of the rehabilitation, and for high intensity interval training at the end of the rehabilitation.
Regarding training volume, participants agreed that long COVID-19 inpatients should train at least 30 minutes/day and that long-COVID-19 outpatients should train at least 30 minutes 3 times/week.
According to the consensus oxygen saturation, heart rate, dyspnea and clinical signs should be monitored at rest, during exercising, directly after exercising and 2 minutes after having done the exercises. Regarding training intensity assessment, there was a strong agreement (>80%) for the modified Borg scale for all types of training (except for plyometric training).
Assessment and treatment of respiratory problems
Both, assessments, and treatments retained in the consensus depended on the type of respiratory problem. For dyspnea for example, participants consented on using the modified Borg Scale, the mMRC scale, the 6 Minute Walk Test, and the self-reported chronic respiratory questionnaire whereas for hypoxemia an assessment of the blood saturation (SP02) and an arterial blood gas analysis were retained. In a similar way, all participants agreed that dyspnea should be treated by breathlessness management techniques and by graded activity with an increase in activity demand, whereas an oxygen supplementation reached the major consensus for treating hypoxemia. Nevertheless, certain training strategies, such as an endurance training, were suggested for taking care of different respiratory problems (dyspnea, hypoxemia, pulmonary fibrosis). Table 5 presents all assessments and treatments according to all specific respiratory problems.
Table 5: Assessment and treatment of respiratory problems in long COVID-19 patients.
|
|
ASSESSMENT |
TREATMENT |
|
Dyspnea
|
• modified Borg Scale (0-10) (100%) • mMRC scale (82%) • 6 Minute Walk Test (75%; 83%) • Chronic Respiratory Questionnaire (CRQ) (75%; 79%) |
• Breathlessness management techniques (100%) • Graded activity with an increase in activity demands (100%) • Continuous endurance training (90%) • Breathing exercises (81%) • Respiratory muscles training (81%) • Positioning instructions (81%) • Relaxation exercises (76%; 76%) • Muscle endurance training (71%; 78%) |
|
Hypoxemia
|
• Measure of SPO2 (100%) • Arterial blood gas analysis (80%) |
• O2 supplementation (95%) • Positioning techniques (85%) • Endurance training (81%) • Interval training (71%; 88%) • Instruction of breathing techniques (76%; 83%) |
|
Pulmonary obstruction
|
• Pulmonary auscultation (90%) • Measure of SP02 (71%; 83%) • Spirometry test (added; 81%) |
• Positioning techniques (85%) • Mobilizing secretions techniques (e.g. acapella) (85%) |
|
Hyperventilation |
• Number of breaths per minute (75%; 94%) |
• Calming breathing techniques (90%) |
|
Pulmonary fibrosis
|
|
• Endurance training (68%; 100%) • Interval training (63%; 89%) |
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
\
Assessment and treatment of strength deficits
Items that reached consensus for assessment and treatment of strength deficits are presented in Table 6. Both, assessments, and treatments retained in the consensus depended on each type of strength deficit. Certain training types were suggested for taking care of different strength deficits. Hypertrophy training was retained for treating muscle mass deficit, muscle power deficit and maximal strength deficit. Muscle endurance training was retained for treating muscle mass deficit, muscle power deficit and muscle endurance deficit. Finally, high intensity interval training was retained for treating muscle power deficit, muscle endurance deficit and reduced rate of force development.
Table 6: Assessment and treatment of strength deficits in long COVID-19 patients
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
|
|
ASSESSMENT |
TREATMENT |
|
Muscle mass deficit
|
|
• Hypertrophy training (95%) • Muscle endurance training (86%) |
|
Muscle power deficit
|
• Hand Grip Strength Test (89%) • Manual Muscle Testing (0-5) (81%) • Strength test with a Dynamometer (75%; 93%) • 1-Minute Sit-to-Stand Test (74%; 88%) |
• Hypertrophy training (80%) • High intensity interval training (71%; 89%) • Muscle endurance training (67%; 72%) • Maximal strength training (67%; 76%) |
|
Muscle endurance deficit
|
• 6 Minute Walk Test (67%; 89%) • 1-Minute Sit-to-Stand Test (74%; 94%) |
• Muscle endurance training (100%) • Continuous endurance training (89%) • High intensity interval training (70%; 78%) |
|
Maximal strength deficit
|
• Strength test with a Dynamometer (88%) • Measure of 1-Repetition-Maximum (1RM) (95%) |
• Hypertrophy training (94%) • Maximal strength training (89%) |
|
Reduced rate of force development |
|
• Balance training (85%) • High intensity interval training (75%; 71%) • Plyometric training (75%; 77%) |
Assessment and treatment of joint mobility restrictions
Items that reached consensus for assessment and treatment of joint mobility restrictions are presented in Table 7. According to the participants, joint mobility restrictions should be assessed by measuring passive and active range of motion and should be treated with active/active-assistive mobility exercises, passive mobilization, manual therapy and stretching.
Table 7: Assessment and treatment of joint mobility restrictions in long COVID-19 patients
|
|
ASSESSMENT |
TREATMENT |
|
Joint mobility restrictions |
• Measure passive and active range of motion (86%) |
• Active/active-assistive mobility exercises (100%) • Passive mobilization (90%) • Manual therapy (85%) • Stretching (81%) |
Number in brackets represents the rate of agreement after the 2nd round
Assessment and treatment of balance deficits
Items that reached consensus for assessment and treatment of balance deficits are presented in Table 8. Both, assessments, and treatments retained in the consensus depended on each type of balance deficit. All participants agreed that walking aids should be provided/adapted in case of balance deficits. All participants also agreed that perturbed reactive postural adjustments should be treated by training protective steps and that reduced gait stability should be treated by gait training.
Table 8: Assessment and treatment of balance deficits in long COVID-19 patients.
|
|
ASSESSMENT |
TREATMENT |
|
Static balance deficit
|
• Single leg stance test (90%) • Tandem stance test (90%) • Berg Balance Scale (84%) |
• Proprioceptive exercises (85%) • Dynamic balance exercises with variations (head movements, eyes closed, uneven surfaces, ...) (85%) • Static balance exercises with resistance on different body parts (79%; 88%)
In case of static balance deficits, the following progression could be used: sitting balance training; then standing balance training with movements of the extremities and of the head; then standing balance training with eyes closed; then standing balance training on an unstable plane (90%) |
|
Perturbed sensory orientation |
• Placing test (67%; 83%) |
• Sensory orientation training (eyes closed, stand on different surfaces, head movements, ...) (76%; 94%) |
|
Perturbed reactive postural adjustments
|
• Mini-BESTest (79%; 85%) |
• Training of protective steps (100%) • Balance training (100%) • Reactive postural adjustment exercises (94%) • Exercises with external perturbations (87%) • Stability exercises (87%) |
|
Reduced gait stability |
• Timed up and Go (95%) • Short-Physical-Performance Battery Test (SPPB) (92%) • Tinetti (88%) • Berg Balance Scale (84%) • Dynamic Gait Index (79%; 100%) • mini-BESTest (77%; 83%) |
• Gait training (combined with head movements, dual tasks, ...) (100%) • Static and dynamic balance training (95%) • Functional training (ADL) (95%) • Counseling for home environment (95%) • Muscle endurance training (68; 76%)
|
|
In case of balance deficits, walking aids should be provided/adapted (100%) |
||
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round
Management of other disorders
Items that reached consensus for the management of other disorders are presented in Table 9. The results showed that the physiotherapy treatments should be adapted according to the patient's disorders. The following assessments could be used: the Borg Scale to assess fatigue; the Hospital Anxiety and Depression scale and the EQ-5D to assess anxiety; and the hospital Anxiety and Depression scale to assess stress. In case of anxiety, dysphagia and edema, patients should be referred to a specialist.
Table 9: Management of other disorders in long COVID-19 patients.
Items in italics are those retained after the 3rd round; the first percentage is that from the 2nd round and the second is that obtained after the 3rd round.
|
FATIGUE |
|
• Advice regarding pacing, planning, prioritization, and energy conservation should be given to treat fatigue (100%) • Communication with the interdisciplinary team is very relevant in case of fatigue (95%) • Continuous endurance training should be performed to treat fatigue (95%) • Muscle endurance training should be performed to treat fatigue (95%) • Graded activity should be performed to treat fatigue (90%) • Adapting the therapeutic program (intensity, duration, and resting time) is a good way to reduce fatigue (90%) • Using the Borg Scale is a good way to assess fatigue (86%) |
|
ANXIETY |
|
• Hospital Anxiety and Depression scale should be used to assess anxiety (100%) • Communication with the interdisciplinary team is important if the patient is anxious (100%) • Patient self-confidence should be reinforced if the patient is anxious (95%) • Focus should be put on active listening if the patient is anxious (90%) • Focus should be put on communication if the patient is anxious (90%) • Focus should be put on patient possibilities and resources to reduce anxiety (90%) • Relaxing breathing techniques should be used to reduce anxiety (86%) • EQ-5D questionnaire should be used to assess anxiety (70%; 73%) • Post-COVID-19 patients should be referred to a specialist in case of anxiety (65%; 94%) |
|
DYSPHAGIE |
|
• Patients should be referred to a specialist (100%) |
|
STRESS |
|
• Relaxation should be done to treat stress (84%) • Hospital Anxiety and Depression scale should be used to assess stress (69%; 82%) |
|
EDEMA |
|
• In case of oedema, post-COVID-19 patients should be referred to a specialist (79%; 94%) |
|
DIZZINESS |
|
• The therapist should be very attentive to sudden changes in position (100%) • Dizziness should be treated with ramped verticalization (80%) |
|
COGNITIVE DEFICITS |
|
• Complexity of exercises should be adapted (100%) • Exercises should be given to the patient in written form (with pictures, texts, ...) (58%; 78%) |
|
DISORIENTATION |
|
• In case of disorientation, post-COVID-19 patients should be questioned about the place where they are located, the location of their room, the time etc. during Physiotherapy treatment (76%; 81%) |
|
ATTENTIONAL DEFICITS |
|
• Complexity of exercises should be adapted (100%) • Short instructions should be privileged (100%) • Dual task exercises (50%; 73%) |
|
FEELINGS OF STIGMATIZATION |
|
• Long COVID patient’s education (e.g., information about the virus) is very important (90%) |
Discussion
The present Delphi study allowed us to summarize the most observed impairments reported by physiotherapists in long COVID-19 patients and to find a consensus on which physiotherapy assessment and treatment to recommend for each category of impairment.
The most frequently observed impairments in long COVID-19 patients by physiotherapists are pain, reduction in general physical fitness and respiratory problems. More than 60% of physiotherapists also reported strength deficits, fatigue, increased risk of fall, joint mobility restrictions and balance deficits in their patients. Our study is the first to identify the disorders observed by physiotherapists in long COVID-19 patients. Other studies also documented disorders in long COVID-19 patients but using other methods to collect the data and found similar results to ours7, 22-24.
Assessment
Regarding assessment of long COVID-19 patients, the 6 Minute Walk Test seemed to be essential. It was retained by the participants for assessing general physical fitness, dyspnea, and muscle endurance deficit in long COVID-19 patients. This is in line with the study from Zhao et al.25 who also recommended to use the 6 Minute Walk Test to assess aerobic exercise capacity. For pain assessment, the use of the NRS and the use of the VAS were retained for all types of pain. These two scales seem to be very frequently used in physiotherapy, certainly because of their easy use. Regarding the assessment of respiratory problems, Zhao et al.25 suggested to measure maximum inspiratory pressure and maximal expiratory pressure, two tests which are common to assess respiratory muscles strength26. These tests were not retained in our consensus paper, probably because we did not ask the participants to indicate how they assess the strength of the respiratory muscles. Regarding assessment of muscle strength deficits in long COVID-19 patients, assessments retained in our paper depended on the type of strength deficit to be assessed. For muscle power deficit, the participants retained among others the manual muscle testing which was also proposed by Zhao et al.25 to assess muscle strength. Regarding joint mobility restrictions, our results indicated that they should be assessed by measuring passive and active range of motion. These results agree with those of Zhao et al.25. For balance deficit, assessments retained in our paper depended on the type of balance deficit to be assessed. For the assessment of static balance deficit and of reduced gait stability, participants retained among other the Berg Balance Scale, as also suggested by Zhao et al.25.
Treatment
Regarding physiotherapy management of long COVID-19 patients, physical activity, graded activity, and active mobilization reached the strongest agreement for the treatment of all types of pain. In addition, counseling seemed to be important in pain treatment since it was retained in the consensus for treating muscle pain, nerve pain and skin pain. For the treatment of reduced general physical fitness, participants agreed that muscle endurance training and continuous endurance training should be performed from the beginning to the end of the rehabilitation. These results agree with those of Zhao et al.25 who recommended progressive aerobic exercises so that patients can return to their pre-illness level and regain their place in society and with those of Smondack et al.27 who reported that rehabilitation should contain continuous or interval endurance training (walking, cycloergometer, etc.) and resistance training27. For respiratory problems treatment, breathing exercises/instruction of breathing techniques were retained in our consensus for treating dyspnea, hypoxemia, and hyperventilation. These results agree with those of Curci et al.28 who also recommended the inclusion of breathing exercises such as chest-abdomen coordination exercises and thoracic expansion exercises in respiratory rehabilitation of long COVID-19 patients. Respiratory techniques are also recommended by Liu et al. for post-acute COVID-19 patients. These authors reported that such exercises combined with group psychological interventions decrease anxiety and sleep disorders29. It was also shown that a 6-week respiratory rehabilitation program including among others respiratory muscle training, cough exercise, and diaphragmatic training improved respiratory function and quality of life and reduced anxiety in patients with COVID-1930. Our results also agree with those of Zhao et al.25 who suggested body management and improvement of the respiratory rhythm in case of dyspnea. In addition, in our consensus, endurance training was retained for treating dyspnea, hypoxemia and pulmonary fibrosis; interval training was retained for treating hypoxemia and pulmonary fibrosis; and graded activity was retained for treating dyspnea. Active therapy seems therefore very important in the treatment of respiratory problems, as also suggested by Zhao et al.25. These authors reported that aerobic exercises (for example walking, jogging, or swimming) with a progressive increase in duration and intensity should be performed for the respiratory rehabilitation of patients with COVID-1925. For the management of pulmonary congestion, participants retained positioning techniques and mobilizing secretions techniques, which were also recommended by Zhao et al.25 and by Curci et al.28. In addition, Zhao et al.25 recommended cough training, which was not retained in our consensus but was also recommended by Liu et al.30. Regarding the treatment of joint mobility restrictions active/active-assistive mobility exercises, passive mobilization, manual therapy and stretching were retained in our consensus. These results are in line with the recommendations of Curci et al.28 who in addition to our results separated their recommendation and suggested for an early rehabilitation of post-acute COVID-19 patients with a FiO2 between 40 and 60%, stretching, passive, and active-assistive exercises to prevent tendon retraction and for patients with a FiO2 between 21 and 40% active exercises at bedside to recover mobility.
For balance deficit treatment, according to our results, treatment should be adapted to the type of balance deficit observed in the patient. Participants retained different type of balance exercises to treat static balance deficits, perturbed reactive postural adjustments and reduced gait stability. These results agree with those of Zhao et al.25 who recommended performing balance training during physiotherapy sessions, for example with hands free exercises or using a balance device. Also, the recommendations of Curci et al.28 are in line with our findings by suggesting static and dynamic balance exercises, such as one-legged stance. These authors also recommended exercises for fall prevention, including muscles strengthening and low intensity exercises for limb and trunk muscles, and walking training28, as suggested in our consensus.
Monitoring
Concerning treatment monitoring, participants agreed that oxygen saturation, heart rate, dyspnea and clinical signs should be monitored at rest, directly after exercising, during exercising and 2 minutes after having done the exercises. These results are in line with those of Barker-Davies et al.31 who recommended to monitor heart rate and pulse oximetry during treatment of respiratory symptom. Other authors suggested measuring exercise saturation during tests such as the 1-Minute Sit-to-Stand Test, the 40-step walk test or during home observation16. In addition to our results, authors also recommended to monitor blood pressure31.
Training modalities
Concerning training volume, in our study, participants agreed that in case of reduced general physical fitness, long COVID-19 inpatients should train at least 30 minutes each day and that long COVID-19 outpatients should train at least 30 minutes 3 times/week. These results are in line with those of Smondack et al.27 who recommended at least 3 sessions of exercise rehabilitation per week for outpatients, either at home or in the physiotherapy practice and with those of Zhao et al.25 who recommended a volume of 20 to 30 minutes of exercises 3 to 5 times a week. Concerning muscle strengthening modalities, in our consensus, the recommended volume depended on the type of training performed. For hypertrophy training, participant retained a volume of 3-4 sets of 8-12 repetitions. These results are in partial agreement with those of Zhao et al.25 who also recommended 8-12 repetitions for each muscle group, but only 1-3 sets, with a rest of 2 minutes between each set.
Regarding intensity assessment during the treatment of reduced general physical fitness, the use of the modified Borg scale reached a strong agreement for all types of training (except for plyometric training). Polastri et al.32 also reported that the modified Borg scale, which is easy to implement, could be used to define exercise intensity in patients suffering from COVID-19. For recommended intensity, results of our consensus depended on the type of training and we did not interview the participants about the progression of the intensity. However, in the literature, Barker-Davies et al.31 suggested that pulmonary rehabilitation in long COVID-19 patients should be started at a low exercise intensity (≤3 METs or equivalent), especially for patients who are receiving supplemental oxygen. They also reported that the progression of intensity should be based on the patients' symptoms31. Regarding muscle strengthening, Zhao et al.25 recommended for patients suffering from COVID-19 a progressive resistance training with an intensity increase of 5 to 10% per week.
Management of other disorders
Other disorders, which are common in long COVID-19 patients but are not necessarily the direct reason for a physiotherapy consultation, must be identified by the physiotherapist at the time of the anamnesis and then considered during the treatment. A survey conducted by Singh et al. highlighted that a broader approach than the one used in standard pulmonary programs should be used in the assessment of long COVID-19 patients15. The authors stated that this should include an assessment of post-traumatic stress disorder and fatigue15. In our consensus, participants agreed that fatigue could be assessed with the Borg Scale and they retained in the consensus that anxiety and stress should be assessed with specific questionnaires. On their side, Kalirathinam et al.13 reported that an assessment of quality of life should be done with the Health-Related Quality of Life Assessment and Interventions in patients suffering from COVID-19. Patient’s education and counseling seems also have an important place in the management of these disorders31, 33. In our consensus, participants underlined the necessity of a broader approach and stated that patient’s education is very important in case of feelings of stigmatization and that communication is essential if the patient is anxious. They also agreed that advice regarding pacing, planning, prioritization, and energy conservation should be given in case of fatigue. In addition, other approaches that were not revealed in our consensus but are reported in the literature seem to be important. According to Demeco et al.33, patients should be motivated to actively participate in social and family activities33. In addition, Smondack et al.27 reported that nutritional, emotional, and social support should be offered to patients as needed. Finally, authors reported that management of mental disorders must also be implemented14 and that, if necessary, COVID-19 patients should be referred to a psychologist25.
In our consensus, there were no sections that focused on daily life activities. However, given the variety of symptoms that long COVID-19 can produce, it is very likely that affected patients will experience limitations in their daily activities. The authors therefore recommend assessing them with the International Physical Activity Questionnaire (IPAQ), with the physical activity scale for the elderly (PASE), with the Barthel index or with the Extra Short Musculoskeletal Function Assessment13, 25.
Treatment precautions
In our Delphi study, we did not inquire about precautions to be taken during physiotherapy treatment. However, it was reported in the literature that health care professionals should take some precautions when treating long COVID-19 patients25, 27, 28. Zhao et al.25 reported that long COVID-19 outpatients should not be allowed to perform exercises if (1) heart rate exceed 100 beats/min, (2) blood pressure is lower than 90/60mmHg or higher than 140/90mmHg, and (3) SpO2 is lower than 95%. Furthermore, long COVID-19 patients should immediately stop exercise in case of fever (over 37.2°), increased respiratory complaints or increased fatigue, if it does not decrease after rest25. In their early rehabilitation treatment protocol for post-acute COVID-19 patients, Curci et al. recommended stopping the treatment in case of major fever, increased dyspnea, tachypnea (more than 30 breaths per minute), decreased oxygen saturation (more than 4%) and signs of respiratory distress28. Zhao et al.25 reported the doctor should be consulted if any of the following symptoms appear: chest tightness, chest pain, dyspnea, severe cough, dizziness, headache, blurred vision, heart palpitations, profuse sweating, and unstable gait. Finally, Smondack et al.27 recommended performing cardiopulmonary exercise testing (CPET) or a cardiac stress test to identify possible contra-indications to rehabilitation. If these tests are not possible, the 6 Minute Walk Test or the 6-minute stepper test34 are recommended.
Strengths and limitations
The fact that one of the inclusion criteria was that the physiotherapists had to have treated at least 10 long COVID patients is a main limitation since this number is relatively low. But requiring a higher number of treated patients would have massively limited our recruitment field at the time the study was conducted. In addition, it has to be noted that the Delphi study design aims to collect opinions and/or to get a consensus35 but do not allow to come up with treatment recommendations. The results presented in this study should therefore be interpreted with caution. They are only the opinions of physiotherapists at a given time. Further robust clinical trials should therefore be performed to investigate the effects of suggested treatments on long COVID-19 patients. Another limitation is the fact that we don't know exactly how long after the infection the physiotherapy treatments started. However, we do know that patients came to physiotherapy on average 4.56 weeks after discharge of the intensive care unit. An additional limitation is the low number of participants and the fact that the number of participants has been reduced from 34 in the first round to 24 in the third round. This may be because the questionnaire was relatively long, which may have discouraged some people from participating. In addition, at the time of the study, the physiotherapists were very occupied with the large number of patients to be treated and may not have participated in all rounds due to time constraints. Another limitation is that not all European countries were represented by participants and that a significant proportion of the participants come from Switzerland. However, we were able to collect the opinions of participants working in different fields of physiotherapy (musculoskeletal, cardiorespiratory, neurology) and in different types of settings (hospital, practice, research), which allowed us to obtain a global view of the situation of long COVID-19 patients in physiotherapy. Finally, another limitation is the wide variation in the number of patients treated during the first round, that varied between 0 and 300 long COVID-19 patients already treated. This could be explained by the fact that a small number of participants were not working in the clinics but in research and therefore did not directly treat long COVID-19 patients. However, the inclusion of both researchers and clinicians also represents a strength of the study since it allowed to obtain a very complete overview of the management of long COVID-19 patients in physiotherapy. Another strength of our study is that it is the first published consensus providing very practical and concrete information on the management of long COVID-19 patients in physiotherapy. This consensus contains clear recommendations regarding the assessment, treatment, and monitoring of long COVID-19 patients and does not focus on only one type of symptom but considers the management of a set of impairments frequently observed by physiotherapists, which had never been done before. However, it is important to remember here that the management of long COVID-19 patients is complex and that a multidisciplinary approach is necessary in order for a complete therapy to be implemented36.
Needs for the future
Because the first round was conducted at the end of the first wave in September 2020, participants still had limited experience with long COVID-19 patients. It would be interesting to check if participants still agree with this consensus paper in the near future. In addition, it would be relevant to conduct focus groups so that physiotherapists could discuss the reasons why certain assessments, treatments and monitoring were not included in the consensus. At the same time, given that the results are very comprehensive, it would be interesting to create focus groups to prioritize the assessments, treatments and monitoring to be used and to define in which case which assessment/assessment/monitoring should be performed. Finally, focus groups would also be useful to define the assessment and treatment to be implemented for the categories in which no consensus was found in our study.
Conclusion
Our study highlighted the diversity of symptoms, respectively impairments, observed by physiotherapists in long COVID-19 patients and allowed to create a consensus on the assessments and treatments to be preferred for each type of impairment. Given the diversity of disorders that can occur or persist after a COVID-19 infection, a complete anamnesis is essential to identify which assessments and then which treatments should be implemented. Our results showed that in general, active treatment should be preferred for most of the impairments for which long COVID-19 patients consult a physiotherapist. In addition, other disorders, such as anxiety, stress and feelings of stigmatization that are common in patients suffering from long COVID-19 should also be carefully taken into consideration during physiotherapy treatment.
Declarations of interest
The authors declare no conflict of interest.
Acknowledgement
The authors sincerely thank all participants of the Delphi.
References
- Sohrabi, C., et al., World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg, 2020. 76: p. 71-76.
- Esakandari, H., et al., A comprehensive review of COVID-19 characteristics. Biol Proced Online, 2020. 22: p. 19.
- Carda, S., et al., The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician's view. Ann Phys Rehabil Med, 2020. 63(6): p. 554-556.
- Lopez, M., et al., COVID-19 Guide for the Rehabilitation Clinician: A Review of Nonpulmonary Manifestations and Complications. Am J Phys Med Rehabil, 2020. 99(8): p. 669-673.
- Greenhalgh, T., et al., Management of post-acute covid-19 in primary care. BMJ, 2020. 370:m3026: p. 1-8.
- Sudre, C.H., et al., Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. MedRxiv [preprint], 2020.
- Carfì, A., R. Bernabei, and Landi., Persistent Symptoms in Patients After Acute COVID-19. JAMA, 2020. 324(6): p. 602-603.
- NICE (National Institute for Health and Care Excellence), COVID-19 rapid guideline: managing the long-term effects of COVID-19. NICE guideline, 2020.
- Halpin, S.J., et al., Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol, 2021. 93(2): p. 1013-1022.
- Hanson, S.W., et al., A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv, 2022.
- Lee, A.J.Y., et al., Clinical course and physiotherapy intervention in 9 patients with COVID-19. Physiotherapy, 2020. 109: p. 1-3.
- Nasserie, T., M. Hittle, and S.N. Goodman, Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA network open, 2021. 4(5): p. e2111417-e2111417.
- Kalirathinam, D., R. Guruchandran, and P. Subramani, Comprehensive physiotherapy management in covid-19 – a narrative review. Scientia Medica, 2020. 30(1).
- Spruit, M.A., et al., COVID-19: Interim Guidance on Rehabilitation in the Hospital and Post-Hospital Phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force. Eur Respir J, 2020.
- Singh, S.J., et al., British Thoracic Society survey of rehabilitation to support recovery of the post-COVID-19 population. BMJ Open, 2020. 10(e040213).
- DeMars, J., et al., What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation, 2022: p. 1-4.
- Yan, Z., M. Yang, and C.-L. Lai, Long COVID-19 syndrome: a comprehensive review of its effect on various organ systems and recommendation on rehabilitation plans. Biomedicines, 2021. 9(8): p. 966.
- Swarnakar, R. and S.L. Yadav, Rehabilitation in long COVID-19: A mini-review. World Journal of Methodology, 2022. 12(4): p. 235.
- Skulmoski, G.J., F.T. Hartman, and J. Krahn, The Delphi Method for Graduate Research. Journal of Information Technology Education, 2007. 6: p. 1-21.
- Creswell, J.W. and V.L. Plano Clark, Mixed Methods Research. SAGE Publications ed. 2018, Los Angeles : SAGE.
- Minkman, M., et al., A quality management model for integrated care: results of a Delphi and Concept Mapping study. Int J Qual Health Care, 2009. 21(1): p. 66-75.
- Goertz, Y.M.J., et al., Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res, 2020. 6: 00542-2020: p. 1-10.
- Mandal, S., et al., 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax, 2020. 0: p. 1-3.
- Negrini, F., et al., Rehabilitation and COVID-19: Update of the rapid living systematic review by Cochrane Rehabilitation Field as of April 30, 2021. European journal of physical and rehabilitation medicine, 2021. 57(4): p. 663-667.
- Zhao, H.M., et al., Recommendations for respiratory rehabilitation in adults with coronavirus disease 2019. Chin Med J (Engl), 2020. 133(13): p. 1595-1602.
- Schoser, B., et al., Maximum inspiratory pressure as a clinically meaningful trial endpoint for neuromuscular diseases: a comprehensive review of the literature. Orphanet J Rare Dis, 2017. 12(1): p. 52.
- Smondack, P., et al., Kinésithérapie et COVID-19 : de la réanimation à la réhabilitation à domicile. Synthèse des recommandations internationales. Rev Mal Respir, 2020. 37(10): p. 811-822.
- Curci, C., et al., Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur J Phys Rehabil Med, 2020. 56(5): p. 633-641.
- Liu, Y., et al., Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychology, Health & Medicine, 2022. 27(2): p. 333-342.
- Liu, K., et al., Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract, 2020. 39.
- Barker-Davies, R.M., et al., The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med, 2020. 54(16): p. 949-959.
- Polastri, M., et al., Recommendations from scientific/professional societies: an essential support for physiotherapy in patients with COVID-19. International Journal of Therapy and Rehabilitation, 2020. 27(4): p. 1-3.
- Demeco, A., et al., Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res, 2020. 48(8): p. 300060520948382.
- Borel, B., et al., An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clinical Rehabilitation, 2010. 24: p. 82–93.
- Trevelyan, E.G. and P.N. Robinson, Delphi methodology in health research: how to do it? European Journal of Integrative Medicine, 2015. 7(4): p. 423-428.
- Joshee, S., N. Vatti, and C. Chang. Long-term effects of COVID-19. in Mayo Clinic Proceedings. 2022. Elsevier.
