A Single Session of Spinal Decompression with Oscillation and Videofluoroscopy
Richard E. Busch III D. C1*, Prahlad G Menon2, Sergey Leo Sorin, M.D., DABFM3
1Indiana University, Parker University, Dallas, TX
2Bioengineering, University of Pittsburgh, Pittsburgh, PA
3International Institute of Holistic Medicine, 2840 E. Chestnut Expy, Springfield, MO
Abstract
Background: Computerized spinal decompression using the intervertebral differential dynamics (IDD) therapy protocol has achieved 86–92% positive results in reducing back pain. There are many causes of back pain, and one of the most common is a degenerative disc. The etiology of a degenerative disc is not completely understood, but it can be related to acute injuries, repetitive stress, nutrition, genetic factors, and oxidative stress1. Standard of care may include physical therapy or manipulation to introduce movement to the spinal vertebrae. IDD Therapy® uses a calculated, sinusoidal, logarithmic primary waveform to separate the spinal vertebrae. More recent studies have shown that the addition of a secondary waveform gives a significant increase in efficacy. We observed these effects on the spine during an IDD Therapy® session.
Methods: Images of the intervertebral space were taken by videofluoroscopy during the IDD Therapy® session.
Results: The expected separation of L5-S1 was achieved. We also noted the separation profile of the vertebrae was uniquely uniform despite the graduated pressures, particularly when the secondary oscillation waveform was introduced. L5-S1 separation was 1 mm in size, and the anterior–posterior correlation was significant (p<0.05).
Conclusion: Active oscillatory signaling introduced during the high-tension period of treatment may lead to more compliant muscle re-education and thus enhanced uniform separation of the vertebrae. We believe that IDD Therapy® using Accu-Spina® may achieve 92% positive results because the secondary oscillatory signal induces mechanotransduction of mechanical stimuli into electrochemical activity at the cellular level. Further research will lead to greater confidence and further exploration of mechanotransduction in intradiscal cellular tissues.
Background
The first computer-directed spinal treatment device was invented by Carlos Becerra to target back pain through decompression of the disc2. In 1998, C. Norman Shealy, MD Ph.D., demonstrated an 86% success rate using this non-surgical device. In contrast, lumbar spine surgery fails in an estimated 10–46% of cases following the first surgery, and the success rate diminishes with each consecutive surgery3. The Accu-Spina® uses multiple onboard, looped communication feedback computers and software-driven treatment variations to create algorithms that vary the dynamic force applied to the spine. In 2004 a new technology “System and method for providing decompression modalities using smooth transition signaling and oscillatory signaling at high tension levels for spinal treatment” (Figure 1) was submitted and later awarded a U.S. patent. This introduction of a specific oscillating logarithmic curve was added to each intervertebral differential dynamics (IDD) therapy-enabled device. Concurrently, studies of IDD Therapy® with the Accu-Spina® (using the sinusoidal and oscillation software enhancements) achieved treatment success rates approaching 92%2.
Figure 1: Patent – Mr. Carlos Becerra – North American Medical Corporation. (Source: NAM staff)
The IDD-specific decompression has advantages over routine traction or conventional decompression. Early studies with ordinary traction devices showed that the spinal structure, particularly involving traumatized tissues, does not respond well to aggressive movements. Therefore, the newer patented algorithm employs smooth transition signaling and oscillation to offer a precisely controlled speed, intensity, and duration of every minuscule force transition. This creates a calculated sinusoidal motion effect on the primary waveform (Figure 2)3.
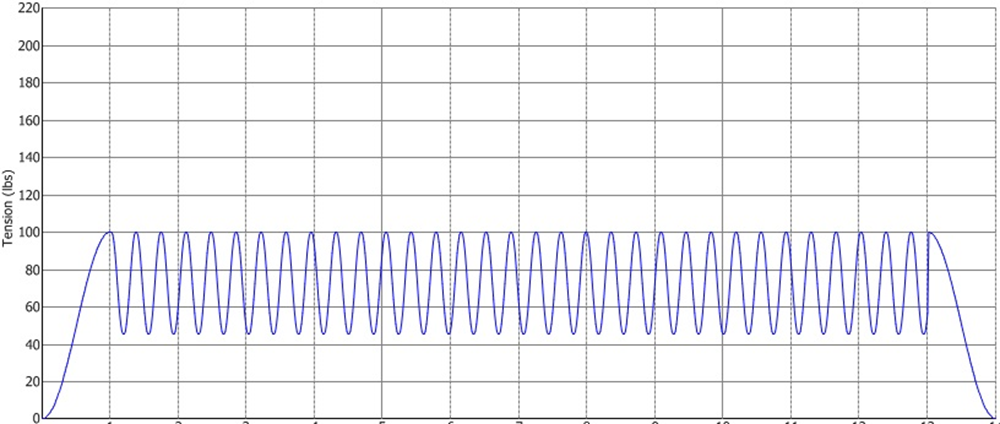
Figure 2: Primary waveform of intervertebral disc distraction therapy on the Accu-Spina® machine. (Source: NAM staff)
IDD Therapy® using the Accu-Spina® system (Figure 3) is a clinically proven, non-surgical approach for treating back pain. It encourages spinal regeneration by correcting the underlying causes of pain for issues such as degenerative disc disease, herniated discs, and sciatica. IDD Therapy® and other conservative treatments far outweigh the risk of spinal surgery, which has a 10–46% failure rate and 10–24% potential side effects4,5. IDD Therapy® can isolate each lumbar vertebra (L1, L2, L3, L4, or L5) and distract the vertebrae surrounding an injured disc by 5 to 7 mm. Treatment for 25 to 30 minutes provides static, intermittent, and cycling forces on the vertebrae and surrounding musculature that may be causing low back pain.

Figure 3:
Accu-SPINA® System device with IDD Therapy® oscillation. (Source: NAM staff)
Accu-Spina® allows for specific mobilization, or distraction, of the targeted spinal segment (in this case, L4 or L5 of the lower back)6. IDD achieves spinal decompression through the application of two waveforms that apply mobilization to the spinal region: a) a primary loading waveform; b) a second higher frequency waveform overlay (i.e., secondary oscillations in addition to the primary waveform currently used in IDD Therapy®). The secondary oscillatory waveform is described as a micro-waveform. This feature could be employed (or not) along with the algorithm, but it is typically introduced only during the high-tension treatment time (i.e., at the peak of the curve), which corresponds to the period during which spinal structures and tissues are at their maximum extension for that treatment session7. According to a 1994 study by Ramos and Martin, these decompressive forces can reduce the intradiscal pressure of the nucleus pulposus to below -100 mm HG during the high-tension cycle of decompression therapy8.
We expected a greater separation of the vertebral bodies at the treatment site when both waveforms are used. This study aimed to establish the value proposition of the secondary waveform called ‘oscillation in optimizing spinal rehabilitation’ over the course of a single session. However, correlation does not imply causation. Therefore, this practice-based study was designed to explain the better outcomes in patients when secondary oscillatory signaling is used in addition to the primary decompression waveform. We decided to observe the treatment “from the inside” by using digital motion fluoroscopy9 to record the targeted spinal vertebrae during IDD Therapy® with the Accu-Spina®.
Materials and Methods
The observed patient was a 51-year-old male of 168.50 cm in height and 61.78 kg in weight. The IDD parameters were as follows: The angle of therapy application was 10 degrees relative to the horizontal plane. A moderate, 2.27 kg of primary distraction force was applied in a calculated sinusoidal waveform (Figure 2). A secondary oscillating waveform was applied in addition to the primary waveform of cyclic loading. This secondary oscillatory waveform offered a higher frequency logarithm over the primary loading waveform by delivering traction to the surrounding muscle tissue to release any muscle spasm (Figure 4). X-ray videofluoroscopy (XVF) (Figure 5) was used to observe the spinal decompression. XVF is a motion x-ray that records 30 radiographs per second and shows continuous x-ray images as a video on a monitor. A baseline image was acquired when no loading was applied. Then, a time-resolved XVF image sequence was recorded in 10-second loops. This gave a total of 13 uniformly spaced cycles throughout the 25-minute session and 11 motion studies. The first loop was gated for 10 seconds to correspond to the peak of the primary waveform of loading and again at the low hold of the cycle. The angle was set at 5 degrees for L5/S1. (An angle of 10 degrees is recommended for L4-L5.)
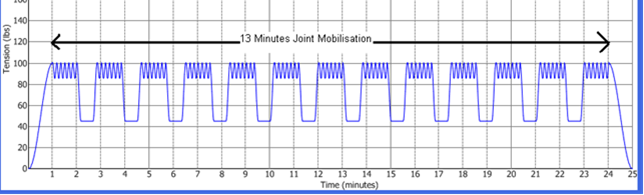
Figure 4:
Oscillations (secondary waveform) of intervertebral disc distraction therapy on the Accu-Spina® machine.(Source: NAM staff)
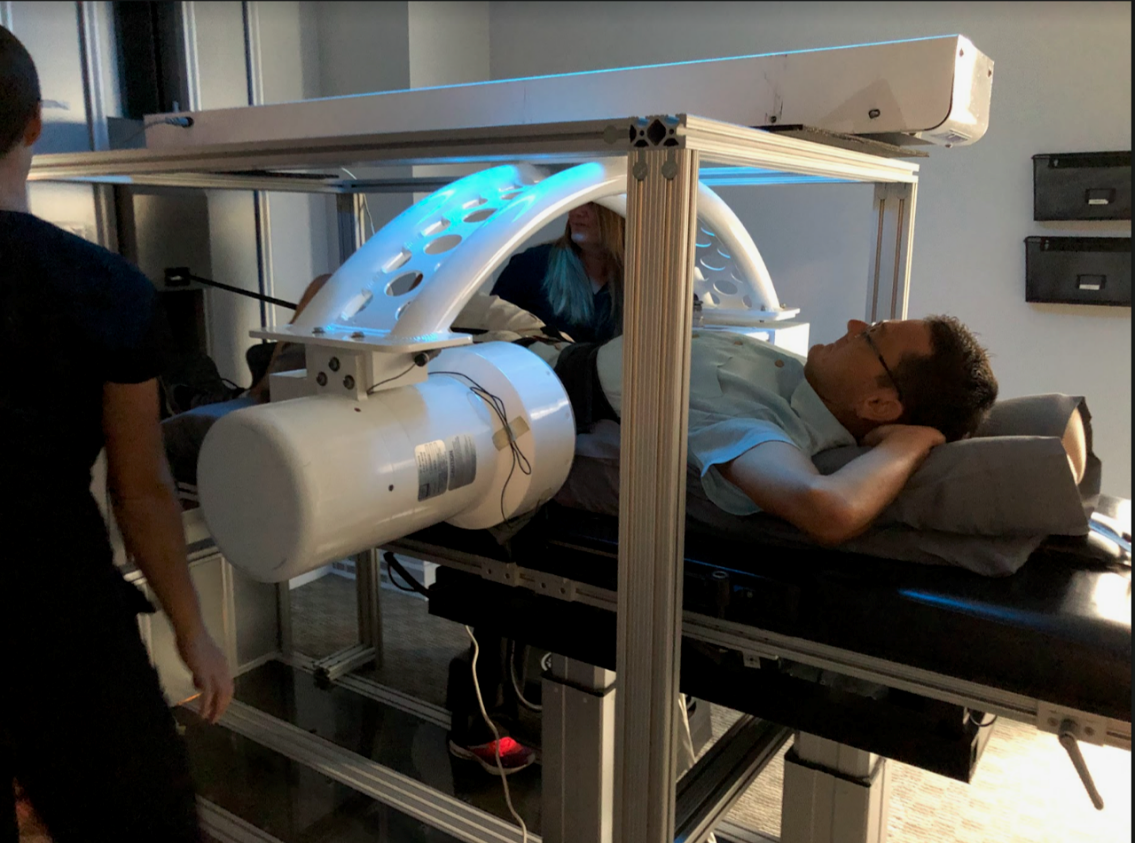
Figure 5: The Accu-Spina® device used in this study was retrofitted with custom hardware to mount the videofluoroscopy camera.(Source: Dr. Busch)
Rigid body registration was performed for consecutive pairs of XVF frames that represented each separate acquisition during the therapy10. The mapping of coordinates from one image frame to the next took the form as illustrated in Figure 6, where Δu represents the translation, in addition to the rotation angle θ, for each frame-pair during the registration process.
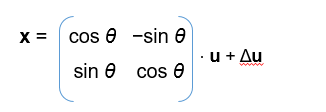
Figure 6: The mapping of coordinates from one image frame to the next, where Δu represents the translation, in addition to the rotation by an angle θ, for each frame-pair, during the registration process.(Source: Developed by Dr. Menon)
The anterior and posterior separations of the L5-S1 vertebral disc space in a single selected frame for each of the 13 fluoroscopy video acquisitions were measured, as well as the baseline. These measurements established the evolution of disc separation as a function of exposure to the therapy. Two independent observers recorded the anterior distances on the left side between the upper bone spurs and the posterior distances on the right side between the upper bone spurs. The mean of these two observations was used in the analysis. We compared the progression of vertebral separations over time, in addition to the separation between specific paired instances of time, to establish the effect of the secondary waveform. Student’s t-test was used to assess statistically significant differences between the vertebral separations. Significance was defined as p<0.05.
The patient underwent one 25-minute IDD Therapy® session. He was diagnosed with an L4/5-disc herniation of 7 mm and was an 8/10 on the visual analog scale for pain (VAS). The patient was placed on a 25-visit treatment regimen over an 8-week period of time. He was treated by IDD Therapy® four times for the first three weeks and three times for the second three weeks. This was followed up by two IDD Therapy® sessions for the last 2 weeks. Upon release, the patient rated his pain as 0–1/10 on VAS.
Results and Discussion
Application of the oscillation waveform along with the primary waveform resulted in a uniquely uniform, gentle separation of vertebral structures and no rotational taxing of the surrounding tissues (Figures 7 and 8). Anterior and posterior separations were correlated significantly (p<0.05), indicative of uniform L5-S1 separation, and our inter-observer variability study showed that the measurements of L5-S1 distances in the anterior and posterior regions of the vertebral column were repeatable and reproducible over time. The magnitude of the observed decompression was approximately 1 mm during the 25-minute IDD Therapy® session under loading conditions of 2.27 kg. These results demonstrated that treatment using the secondary oscillation waveform in addition to the primary waveform can provide a significant benefit over primary decompression alone.
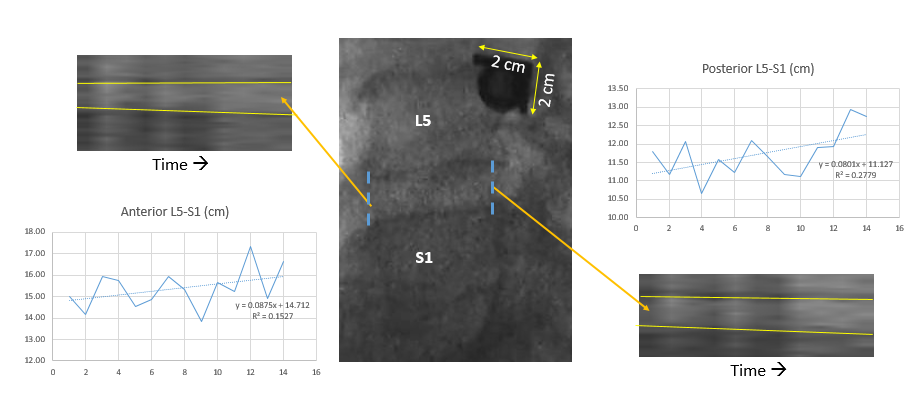
Figure 7: Lumbar separations and corresponding load characteristics recorded via the device treatment screen, videofluoroscopy view of the corresponding separation, and measurements.(Source: Developed by Dr. Menon on the Accu-Spina® machine)
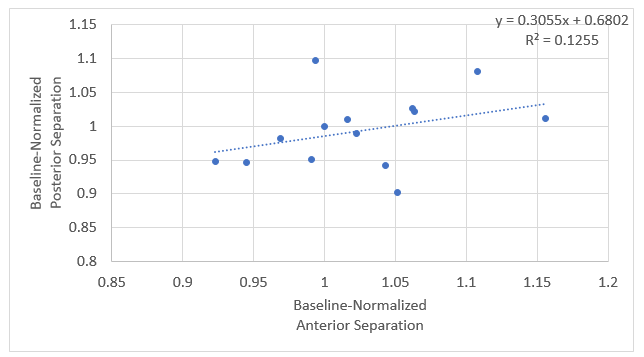
Figure 8: Anterior separation vs. posterior separation.(Source: Developed by Dr. Menon)
Uniform separation of the vertebral bodies has several advantages compared to procedures that result in a less uniform or non-uniform separation. Prior spinal decompression studies have shown “distraction decompression over time” reduced disc herniation and improved hydration after multiple sessions11, we achieved a significant distraction from a single session of therapy. We also noted positioning uniformity was greater than with primary decompression alone. These advantages include more efficient biomechanics and increased overall space between the vertebrae. In addition, there is an inverse relationship between separation and intradiscal pressure. Negative intradiscal pressure promotes the diffusion of water, oxygen, and nutrients into the vertebral disc area, which rehydrates a degenerated disc and promotes self-healing and rehabilitation. Furthermore, repeated pressure differentials can reduce pressure on vertebral joints and promote the retraction of a herniated nucleus pulposus (the elastic core of an intervertebral disc), thereby relieving low back pain12-14.
The separation achieved in this study is consistent with the literature on spinal decompression therapy8,15-17. We are not aware of any prior study that observed the behavior of vertebral spine segments mobilized by a combination of different dynamic waveforms.
It is important to note that joint tissues are sensitive to their mechanical environment. Therefore, mechanical loading can regulate the development and long-term maintenance of joint tissues18. With advances in technology that allow the measurement of forces on cells and tension within a cell, it has become clear that the role of physical forces is far-reaching beyond what we experience as muscular effort. We know that mechanical forces can alter biological outcomes, even at a cellular level. This is the science of mechanotransduction18.
Forces not only at a muscular level but also at a cellular level are known to affect cell behavior and osmotic changes. Therefore, it stands to reason that variability in forces would yield variability in outcomes19. To understand mechanotransduction in the context of spinal dysfunction treated using a physical medicine modality, we used specific, sinusoidal calculations to apply measured forces to the intervertebral structures of the low back. Previous studies using numerous modalities originating with distraction and evolving through manipulation and decompression and more specific algorithms have yielded good to excellent treatment results20-22.
IDD Therapy® utilizes a patented algorithm with clinical study outcomes approaching 92% success rates23. The primary sinusoidal force is delivered to the spine while the patient relaxes in a supine position. A secondary force of a smaller but higher frequency is delivered at the maximum load threshold of each primary sine wave during treatment. This additional force (the sine wave) then layers another calculated physical force, which may or may not be perceived neurologically. However, from the perspective of mechanotransduction theory24,25, this higher frequency physical stimulus may have a physiological effect on the cells in the joint tissues. Notable improvements in treatment outcomes have been observed in studies conducted on patients treated with sinusoidal plus oscillatory signaling26. Therefore, we hypothesize that this unique modality has an algorithmic formula that is optimal for relieving back pain.
The additional waveform applies a differential physical force calculation during the treatment. Therefore, the principle of Hooke’s Law27 raises the question of whether cells can sense these force changes and whether they affect the elasticity of the tissues and tissue cells. The laminae of adjacent vertebrae in both the anterior and posterior medial regions possess collagen and elastin fibers. The synovium and folds of tissues in the joint are richly innervated with mechanoreceptors, proprioceptors, and nociceptors. Differentiating loads would activate nerve endings and modulate signals in the nervous system to initiate or alter cellular dysfunction. In such circumstances, the nervous system is also involved in modulation.
Previous research has shown that all musculoskeletal (MSK) structures display varying degrees of elasticity28. The principles of elastic motion in MSK medicine dictate that the application of an external force (i.e., an IDD Therapy® treatment) would result in MSK structure lengthening. But analysis of the stretch–shortening cycle showed that, except for direct contact injuries, MSK injuries result from an inability to counter the applied forces while lengthening29. Therefore, despite the mechano-sensitive channels that allow physical stimuli to control the flow of molecules across membranes, the application and the modification time of forces on MSK failure may cause the release of osmotic pressure to initiate another signaling pathway.
Cells can sense mechanical stresses and convert them into intracellular signals and biochemical reactions. Wang30 and Schoen, et al.31 later discovered that cells within tissues are subjected to physiological forces, such as fluid sheer stress or mechanical load, which also exert contractile forces on the extracellular matrix32,33.
Thus, intracellular signaling may be involved in the treatment outcomes achieved by oscillation signaling that utilizes a sinusoidal algorithmic force applied to the spine, but further research is needed to establish this relationship. Our observations were from a single angle of application and an applied peak magnitude of distraction force, whereas variations in these parameters may affect the L5-S1 decompression. The hypothesis that physical cues are transformed into a biological response34 that helps the cell adapt to continuous dynamic changes in micro-environmental factors lays a groundwork for exploring the beneficial impact of therapeutic modalities on the MSK system via dynamic specificity.
As we advance into new frontiers of science, we are expanding our knowledge of the possible mechanisms of action of oscillatory signals on biological structures. This may present new approaches in optimizing the beneficial physiological effects of non-surgical decompression treatment, or in this case, advanced IDD Therapy® decompression when oscillatory signaling is added to the protocols for spinal care.
This study was done for one 25-minute IDD Therapy® session. He was diagnosed with an L4/5-disc herniation of 7 mm and was an 8/10 on a VAS. The patient was placed on a 25-visit treatment regimen over an 8-week period of time. He was treated with IDD Therapy® four times during the first three weeks and three times for the second three weeks. This was followed up with two IDD Therapy® sessions the last 2 weeks. Upon release, the patient rated his pain at 0-1/10 on a VAS.
Conclusions
Computerized spinal decompression using IDD Therapy® has shown 86–92% positive outcomes in reducing back pain. This protocol uses a primary waveform to separate the spinal vertebrae. In this study, we used Accu-Spina® to apply a combination of primary and secondary waveforms to the L5-S1 vertebrae and recorded the effects using XVF. During the 25-minute IDD Therapy® session, the patient showed an increase in anterior and posterior separations, resulting in a uniquely uniform, gentle separation of vertebral structures and no rotational taxing of the surrounding tissues. We believe that IDD Therapy® using Accu-Spina® may achieve 92% positive results because the secondary oscillatory signal induces mechanotransduction at a cellular level. This was a single treatment evaluation, and future studies with multiple applications would be beneficial.
Disclosures and Acknowledgments
This research project was self-sponsored. The authors acknowledge North American Medical Corporation for their technical support in this project. Dr. Menon was responsible for the fluoroscopy, methods, and design. Dr. Menon also significantly contributed to the results section. Dr. Sorin provided valuable guidance for the background and discussion. All three authors contributed to the final editing. Each author has reviewed the entire paper.
Conflicts of Interest
None.
References
- Choi YS. Pathophysiology of degenerative disc disease. Asian Spine J. 2009 Jun; 3(1): 39–44. doi: 10.4184/asj.2009.3.1.39. Epub 2009 Jun 30. PMID: 20404946; PMCID: PMC2852042.
- McClure D, Farris B. Intervertebral differential dynamics therapy—a new direction for the initial treatment of low back pain. Eur Musculoskeletal Rev. 2006; 1: 45–47.
- Riehl BD, Park JH, Kwon IK, et al. Mechanical stretching for tissue engineering: two-dimensional and three-dimensional constructs. Tissue Eng Part B Rev. 2012; 18(4): 288–300.
- Daniell JR, Osti OL. Failed Back Surgery Syndrome: A Review Article. Asian Spine J. 2018 Apr; 12(2): 372-379. doi: 10.4184/asj.2018.12.2.372. Epub 2018 Apr 16. PMID: 29713421; PMCID: PMC5913031.
- Castillo H, Chintapalli RTV, Boyajian HH, et al. Lumbar discectomy is associated with higher rates of lumbar fusion. Spine J. 2019 Mar; 19(3): 487–492. doi: 10.1016/j.spinee.2018.05.016. Epub 2018 May 21. PMID: 29792995.
- Zaina F, Tomkins-Lane C, Carragee E, et al. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Jan 29;2016(1):CD010264. doi: 10.1002/14651858.CD010264.pub2. PMID: 26824399; PMCID: PMC6669253.
- Sheaves EG, Snodgrass SJ, Rivett DA. Learning lumbar spine mobilization: the effects of frequency and self-control of feedback. J Orthop Sports Phys Ther. 2012; 42(2): 114–124.
- Chen J, Liu Z, Zhong G, et al. Cyclic stretch enhances apoptosis in human lumbar ligamentum flavum cells via the induction of reactive oxygen species generation. J Spinal Cord Med. 2016; 39(4): 450–454.
- Ramos G and Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg. 1994; 81(3): 350–353.
- Ahmadi A, Maroufi N, Behtash H, et al. Kinematic analysis of dynamic lumbar motion in patients with lumbar segmental instability using digital videofluoroscopy. Eur Spine J. 2009; 18: 1677–1685.
- Thévenaz P, Ruttimann UE, Unser M. A pyramid approach to subpixel registration based on intensity. IEEE Trans Image Process. 1998; 7(1): 27–41.
- Eyerman EL. Simple pelvic traction gives inconsistent relief to herniated lumbar disc sufferers. J Neuroimaging. 1998; 8(2).
- Yeomans S. Spine-Health. IL, USA; Veritas Health, LLC; 2013. Available from: https://www.spine-health.com/treatment/chiropractic/chiropractic-treatments-lower-back-pain.
- Patnaik G. Herald. VA, USA; Herald Scholarly Open Access; 2018. Available from: http://www.heraldopenaccess.us/openaccess/role-of-idd-therapy-in-the-back-and-neck-pain.
- Accu-Spina. IDD Therapy®. GA, USA; North American Medical Corporation; 2019. Available from: https://www.iddtherapy.com/accu-spina/.
- Clarke JA, van Tulder MW, Blomberg SEI, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2007; 2: CD003010.
- Shealy CN and Borgmeyer V. Decompression, reduction, and stabilization of the lumbar spine: a cost-effective treatment for lumbosacral pain. Am. J. Pain Manag. 1997; 7: 63–65.
- Eyerman EL. Simple pelvic traction gives inconsistent relief to herniated lumbar disc sufferers. J Neuroimaging. 1998; 8(2).
- Sun HB. Mechanical loading, cartilage degradation, and arthritis. Ann N Y Acad Sci. 2010; 1211: 37–50.
- Paluch EK, Nelson CM, Biais N, et al. Mechanotransduction: use the force(s). BMC Biol. 2015; 13: 47.
- Gudavalli MR, Olding K, Joachim G, et al. Chiropractic distraction spinal manipulation on postsurgical continued low back and radicular pain patients: A retrospective case series. J Chiropr Med. 2016; 15(2): 121–128.
- Hussain A, Erdek M. Interventional pain management for failed back surgery syndrome. Pain Pract. 2014; 14(1): 64–78.
- Cox JM. Low back pain: mechanism, diagnosis, and treatment. 7th Edition. PA, USA; Lippincott Williams & Wilkins; 2012.
- McClure D, Farris B (2006) Intervertebral differential dynamics therapy—a new direction for the initial treatment of low back pain. Eur Musculoskeletal Rev 1:45–47 (Ref Type: Report).
- Paluch EK, Nelson CM, Biais N, et al. Mechanotransduction: use the force(s). BMC Biol. 2015; 13: 47. Published 2015 Jul 4. doi: 10.1186/s12915-015-0150-4.
- Sun Q, Hou Y, Chu Z, et al. Soft overcomes the hard: flexible materials adapt to cell adhesion to promote cell mechanotransduction. Bioact Mater. 2021; 10: 397–404.
- Egwu MO, Ojeyinka AA, Olaogun MOB. The effect of vertical oscillatory pressure (VOP) on youths and elderly adult low back pain (LBP) intensity and lumbo-sacral mobility. J Jpn Phys Ther Assoc. 2007; 10(1): 17–26.
- Giuliodori MJ, Lujan HL, Briggs WS, et al. Hooke’s law: applications of a recurring principle. Adv Physiol Educ. 2009; 33(4): 293–296.
- Monroy JA, Powers KL, Gilmore LA, et al. What is the role of titin in active muscle? Exerc Sport Sci Rev. 2012; 40(2): 73–78.
- Verrall G, Dolman B. Deducing a mechanism of all musculoskeletal injuries. Muscles Ligaments Tendons J. 2016; 6(2): 174–182.
- Wang N, Butler JP, Ingber DE. Mechanotransduction across the cell surface and through the cytoskeleton. Science. 1993; 260(5111): 1124–1127.
- Schoen I, Pruitt BL, Vogel V. The yin-yang of rigidity sensing: how forces and mechanical properties regulate the cellular response to materials. Annu Rev Mater Res. 2013; 43: 589–618.
- Huxley AF. Muscle structure and theories of contraction. Prog Biophys Chem. 1957; 7: 255–318.
- Martino F, Perestrelo AR, Vinarský V, et al. Cellular mechanotransduction: from tension to function. Front Physiol. 2018; 9: 824.
