Pulmonary Rehabilitation Exercise Assessments and Training Methods for Patients with COPD: A Literature Review
Li Chen1, Jing Su2*
1Department of Nursing, Shantou University Medical College, Guangdong, China
2Director of Department of Nursing, Shantou University Medical College, China
Abstract
Pulmonary rehabilitation (PR) is an important part of the management of COPD, which can reduce symptoms of dyspnea, times of hospitalizations, and improve exercise capacity and health-related quality of patients. As a key element of PR, PR exercise training consists of exercise assessment and training methods. Exercise assessments should include the evaluation of dyspnea, exercise capacity, and health-related quality of life. Following a thorough assessment of patients, individualized exercise training programs, including endurance, resistance, and other exercise training methods, should be developed based on physiologic requirements and individual demands of patients. Although there have been many studies on the types of exercise for patients with COPD, there are still no conclusions about how to develop the best exercise prescription. Choosing the most appropriate methods for patients with COPD to calculate the situation is crucial. Therefore, this review aims to summarize the common methods of exercise assessments and exercise trainings in PR.
Introduction
Chronic obstructive pulmonary disease (COPD) is a respiratory system disease characterized by irreversible airway obstruction and emphysema formation, and its clinical feature is gradually aggravating dyspnea1. Due to the high incidence, disability and mortality of COPD, it will bring different level of activity limitation, psychological barriers and reduced social adaptability to patients, which will greatly affect life quality of patients2. Most patients are prone to dyspnea during daily activities and physical exercise, and the discomfort caused by dyspnea often leads to resistance to participate in physical exercise3. In addition, long-term lack of physical exercise or insufficient exercise will lead to weakness of body muscles. Over time, low-intensity activities can also cause breathing difficulties. In recent years, more and more scholars and clinical experts have realized the importance of exercise training in pulmonary rehabilitation (PR) and it has been considered as the core content of pulmonary rehabilitation program (PRP)4. A large number of studies have shown that PR exercise training can effectively alleviate symptoms of dyspnea in patients with COPD, improve patient's exercise tolerance and health-related quality of life, and reduce times and days of hospitalization. However, PR exercise training, as an important element in the management of COPD, is still in its infancy. Generally, PR exercise training is carried out in a "one size fits all" manner without considering physiologic requirements and individual demands of different patients. Therefore, this review focuses on exercise assessments, exercise training methods, frequency, duration and intensity for patients with COPD.
Pulmonary Rehabilitation Assessments
The American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) first advocated exercise assessments of patients in 1995, and this concept was reinforced in the AACVPR Guidelines for Pulmonary Rehabilitation Programs, published in 20065. In the same year, the American Thoracic Society and the European Respiratory Society (ATS/ERS), in their published Practice Guidelines for Pulmonary Rehabilitation, also recommended the inclusion of patient exercise assessment in clinical practice, including assessments of dyspnea symptoms, exercise capacity, and health-related quality of life (HRQL)6,7. It is important to perform exercise assessments on patients before and after PR exercise training, and the results of it can help optimize the development of care protocols and provide individualized exercise programs for patients to receive better therapeutic interventions.
Assessment of dyspnea symptoms
Patients with chronic lung diseases may have ventilation restrictions during exercise. Therefore, the American College of Sports Medicine (ACSM) believes that the use of age-predicted heart rate to estimate peak oxygen uptake is not entirely appropriate for exercise assessment of patients. It may be necessary to modify the traditional testing protocol based on the dyspnea symptoms and functional status of patients8.
Dyspnea is one of the most common symptoms of patients with COPD. Evaluate and record the level of dyspnea that occurs before, during, and after the patient’s PR exercise training is of great significance, which can help adjust the individualized exercise training program for patients. Table 1 lists some of the commonly used scales for evaluating dyspnea, among which, the modified British Medical Council (mMRC) scale and the Borg scale are now more widely used in clinical practice due to the advantages of fewer items and the convenience of being used by telephone, cell phone, and other communication devices9. The Borg scale is usually used with the 6-minute walk test (6MWT) to better evaluate dyspnea and exercise capacity of patients10. The Visual Analogue Scale (VAS) is only suitable for evaluating dyspnea in a single patient and is not suitable for comparison between several different patients11. The Modified Version of the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ-M) can measure both level of activity-related dyspnea and fatigue in patients with COPD, providing a useful tool for clinical application and study of dyspnea symptoms and functional status12. The Baseline Dyspnea Index/Transformation Dyspnea Index (BDI/TDI) is suitable for evaluating dyspnea in patients and for use during acute changes13. The BODE index, in addition to being an index for evaluating patients' severity grading, it can also be used as a new assessment index for PR14, but it is not yet widely used in clinical practice.
Table 1. Assessment of Dyspnea Evaluation in Patients with COPD
|
Assessment methods |
Introduction |
Function |
|
mMRC9 |
It is divided into 0-4 levels according to the level of activity of the patient when shortness of breath occurs, with higher levels indicating that the patient is more likely to have dyspnea. |
Assess the level of patient's dyspnea. |
|
Borg10 |
It is composed of 0-10 levels from top to bottom, the higher the grade, the more likely the patient is to have shortness of breath. |
Evaluate patient's breathing intensity and dyspnea. |
|
VAS11 |
It consists of a horizontal or vertical segment with a length of 100mm. The description of dyspnea degree is arranged at different positions on the line, and the degree of dyspnea of the patient is reflected by measuring the distance between the patient's markers and the end of "no dyspnea". |
Use visual analogy to reflect and assess patient’s dyspnea. |
|
PFSDQ-M12 |
It is a simplified version of the pulmonary functional status and dyspnea questionnaire (PFSDQ). Contained 40 items, three dimensions: activity, dyspnea, and fatigue. |
Used to evaluate the functional status and dyspnea of patients with COPD. |
|
BDI/TDI13 |
BDI consists of 3 parts: functional impairment, mobility, and effort. Each part is composed of 4 levels; TDI is improved on the basis of BDI, and each part is divided into 7 levels. |
BDI evaluates dyspnea of a patient in a single state, and TDI can show changes in baseline. |
|
BODE14 |
It consists of four scores: body mass index, airflow obstruction, dyspnea symptom and exercise capacity. |
Used to evaluate the severity of patients with COPD and predict the progress and mortality of it. |
Abbreviations: mMRC, modified British Medical Council; VAS, Visual Analogue Scale; PFSDQ-M, Pulmonary Functional Status and Dyspnea Questionnaire; BDI/TDI, Baseline Dyspnea Index/Transformation Dyspnea Index; BODE, body-mass, airflow obstruction, dyspnea symptom and exercise capacity index; COPD, chronic obstructive pulmonary disease.
Assessments of exercise capacity
Cardiopulmonary exercise test (CPET) has always been the gold standard for evaluating exercise capacity of patients with COPD15, and it is also an effective method to assist in the development of PR programs and to evaluate treatment and rehabilitation outcomes. However, CPET requires more advanced equipment, and some hospitals are unable to meet its conditions. Many studies have shown that multiple indicators of simple and easy walking test have a good correlation with CPET, which can assist in testing patient’s exercise capacity. Table 2 lists some commonly used walking tests for patients with COPD, among which, the 6-minute Walking Test (6MWT) is the most commonly used one. Because of its simple execution and does not require special equipment, it is easily accepted by patients, and it also suitable for elderly and frail patients and has more reference value for the evaluation of activities of daily living16. The 6-minute Walking Distance (6MWD) has been strongly associated with important clinical outcomes in patients with COPD, with shorter 6MWD indicating a greater increase in mortality17. However, it is not sensitive to different methods (e.g., Shuttle Walking Test and Straight-line Walking Test) and different environments (e.g., outside the ward and inside the ward), and it has few monitoring indicators, which cannot be analyzed and evaluated systematically in all aspects, so it cannot replace CPET at present18. Also, results of 6MWT may be affected by course layout and track length. However, no such variation has been reported at the Incremental Shuttle Walking Test (ISWT) or Endurance Shuttle Walk Test (ESWT)19. And physiological responses of the ISWT is similar to that of the CEPT. Because walking speed of ISWT is controlled by the recorded signal provided by test taker, making patient's cardiopulmonary function indicators can be evenly incremented so that patients can reach the maximum physiological load of exercise faster20. But it requires pre-recorded signals and it is more difficult to ensure that patients' actions are consistent with the signals, therefore, more studies are needed to verify its reliability. Some studies have shown that the Endurance Shuttle Walk Test (ESWT) is more sensitive in patients with COPD compared with the 6MWT21, but this test needs to be performed after the ISWT, which is more complicated to implement.
Table 2. Assessment of Exercise Capacity in Patients with COPD
|
Assessment methods |
Introduction |
Function |
|
CPET15 |
The test protocol is selected according to the purpose of the study and the patient's physical condition. An appropriate exercise protocol allows the patient to maintain continuous exercise for 6-12 minutes, including incremental power exercise and constant power exercise. |
To understand the interactions and storage capacity between the cardiopulmonary and circulatory systems and to assess maximal exercise capacity. |
|
6MWT16 |
Patients were asked to take a walk on foot to measure the maximum distance they could reach in 6 minutes at the fastest speed they could tolerate. |
Assess exercise endurance. |
|
ISWT20 |
Patient walked back and forth in a corridor with a length of 10 meters, starting at 0.5 m/s and increasing by 0.17 m/s. The distance walked was measured when the patient reached maximum load or experienced discomfort. |
Assess cardiopulmonary function. |
|
ESWT21 |
The maximum ISWT speed of the patient was first obtained according to the ISWT protocol, and then the maximum walking distance that the patient could reach was measured by walking at a steady speed of 85% of the maximum ISWT speed. |
Assess exercise capacity. |
Abbreviations: CPET, Cardiopulmonary exercise test; 6MWT, 6-minute Walking Test; ISWT, Incremental Shuttle Walking Test; ESWT, Endurance Shuttle Walk Test.
Assessment of quality of life in patients with COPD
A large number of studies have been conducted to specifically assess the quality of life of patients with COPD, and many measurement scales have been developed, which are important guides for adjusting clinical caring protocols and developing exercise training programs for PR. Table 3 lists some commonly used clinical quality of life assessment for patients with COPD, including generic scales (SF-36 and EQ-5D) and disease-specific scales (SGRQ, CAT, SOLDQ, CCQ and CRQ).
Generic scales are applicable to all populations and reflects the overall quality of life of the testees. The Short Form of Health Survey (SF-36) has good reliability and validity. It can objectively assess patients' health status and be completed by telephone or other communication devices, but has weak correlation with pulmonary function tests and is less used in clinical trials and practice in patients with COPD22. The EuroQol 5-Dimensional Health Scale (EQ-5D) is a multidimensional scale for evaluating health-related quality of life that developed in Europe. Study of Ge et al.23 has demonstrated that this scale can better reflect health status and quality of survival of patients with COPD.
Disease-specific scale is developed for a specific disease, a specific symptom or a specific population and have a high sensitivity. The St. George’s Respiratory Questionnaire (SGRQ) is currently one of the most widely used specific scales in the assessment of the quality of life of patients with COPD. It can also be used to assess the condition, prognosis and efficacy of patients24. Studies found that the SGRQ had the highest correlation with patients with COPD compared with other scales and can better reflected patients' true condition. However, it has many items, which is too complicated and time-consuming for elderly patients. Compared with SGRQ, COPD Assessment TestTM (CAT) has fewer items, which can be completed more quickly and easily for elderly patients and patients with less education25. Seattle Chronic Obstructive Lung Disease Questionnaire (SOLDQ) has better reliability and is particularly suitable for long-term follow-up studies and analysis quality of life in a large sample of patients with COPD26. However, geographical differences among patients should be considered when using it. Clinical COPD Questionnaire (CCQ) has a few items and is easy to complete. It is usually used in mild to moderate COPD and its use for assessment is less burdensome for patients when they experience deterioration27. Chronic Respiratory Disease Questionnaire (CRQ) is more effective when assessing older patients. It is sensitive to individual changes but less sensitive in patients with milder symptoms or younger age and not suitable for comparison between different populations28.
Table 3. Assessment of Quality of Life in Patients with COPD
|
Assessment methods |
Introduction |
Function |
|
SF-3622 |
Contains 36 questions divided into 8 dimensions, including physiological function, physical function, physical perception, mental state, social function, emotional function and mental health. |
Comprehensive evaluation of patient's physical health and mental health status. |
|
EQ-5D23 |
It is composed of EQ-5D health description system and EQ-5D VAS. EQ-5D health description system is divided into five dimensions, which are motor ability, self-care ability, daily activity ability, pain/discomfort and anxiety/depression. EQ-5D VAS consists of a 20-cm vertical line that reflects the patient's quality of life by measuring the distance between the patient's marker point and the end of the "the best health status in mind". |
Describe the patient's health status and quality of life. |
|
SGRQ24 |
It consists of 50 questions with 3 parts: symptoms (frequency and severity of occurrence), activities (activities that cause shortness of breath or restricted breathing) and impact on daily life (social competence and mental health). |
The gold standard for measuring quality of life and impaired health in patients with respiratory diseases. |
|
CAT25 |
Consisting of 8 items covering various aspects of symptom assessment, mobility, mental health status sleep quality, etc., higher scores represent lower quality of life for patients. |
Simple and reliable for evaluating the quality of life and health status of patients with COPD. |
|
SOLDQ26 |
Contains 29 items measuring 4 aspects of survival quality: motor function, emotional function, satisfaction with treatment and the ability to overcome setbacks. |
Assess patient’s quality of life. |
|
CCQ27 |
It consists of 10 entries divided into 3 dimensions, namely symptoms, physical function and mental health status, with higher scores representing lower quality of life for patients. |
Evaluation of quality of life in patients with COPD and can be used to measure the clinical control of patients. |
|
CRQ28 |
Contains 20 questions divided into 4 sections: dyspnea, fatigue, mood and self-management. |
A recognized standard for evaluating the quality of life of Patients with COPD. |
Abbreviations: SF-36, Short Form of Health Survey; EQ-5D, EuroQol 5-Dimensional Health Scale; SGRQ, St. George’s Respiratory Questionnaire; CAT, COPD Assessment TestTM; SOLDQ, Seattle Chronic Obstructive Lung Disease Questionnaire; CCQ, Clinical COPD Questionnaire; CRQ, Chronic Respiratory Disease Questionnaire; VAS, Visual Analogue Scale; COPD, chronic obstructive pulmonary disease.
Exercise Training
PR exercise training not only enhances muscle aerobic metabolism, increases muscle mass and strength, and improves muscle endurance in patients with COPD, but also reduces lactate levels in patients and decreases minute ventilation and ventilatory demand. Studies29 have confirmed that PR exercise training can increase the exercise tolerance of patients with COPD, relieve their dyspnea symptoms and improve quality of life. Benefits of PR exercise training are not related to the age, disease duration or severity of the disease30, and it is more important to recommend PR exercise training for patients who lack exercise training or have decreased mobility. Exercise training includes various forms; the American College of Sports Medicine (ACSM) recommends endurance exercise training, resistance exercise training and respiratory muscle training for patients with COPD31; the American Thoracic Society and the European Respiratory Society (ATS/ERS) recommend endurance exercise training, resistance exercise training and upper extremity exercise training32; the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) recommends endurance exercise training and resistance exercise training33. Therefore, health professionals need to individualize the exercise training program for each patient. The following is a discussion of exercise training methods in PR.
Methods of exercise training
Endurance exercise training
Endurance exercise training is considered an important part of the PR program. Studies have shown that endurance exercise training can reduce exercise hyperemia, exertional dyspnea and muscle dysfunction in patients with COPD34. Commonly used endurance exercise training includes walking (on a treadmill and on the floor) and cycling (power bikes and regular bikes). A study by Bickford et al.35 in the United States covering 43 states with 283 programs showed that 37% of PR programs used power bicycles, which seemed to be accepted by more patients than other endurance exercise training. Compared with other endurance exercise training methods, bicycles seem to be accepted by more patients because patients were able to convert it into a part of their daily life activities and adhere to it for a long time. However, cycling training often leads to fatigue of the quadriceps, so if a patient desires to improve walking ability, ground walking training may be a better choice.
Resistance exercise training
Patients with COPD are susceptible to varying degrees of muscle atrophy and muscle weakness due to lack of exercise training, and resistance exercise training can help improve muscle strength and symptoms, as well as improve activities of daily living (ADL) and exercise capacity36. In addition to free weightlifting (e.g., dumbbells and shot puts), resistance exercise training can also be performed by using weights on the joints, stretch bands and using one's own body weight to increase the strength load (e.g., stair climbing, squats and sit-ups). Studies37 have shown that multi-joint exercise training (e.g., sit-ups and bench press) is more effective in improving patients' muscle strength than single-joint exercise training. In daily life, patients should be encouraged to perform more multi-joint exercises. The American College of Sports Medicine (ACSM) guidelines on resistance exercise training emphasize the principle of overload, which involves gradually increasing the patient's exercise load over time to maximize muscle strength and endurance31. This can be achieved by increasing the weight load, times of exercises for each group and duration of exercise training and by decreasing the rest time.
Neuromuscular electrical stimulation
Neuromuscular electrical stimulation (NMES) stimulates the phrenic nerve through functional electrical impulses, conducts excitement and plays a similar role to the respiratory center. Currently, commonly used diaphragmatic pacemakers include both in vitro and in vivo. Implantable diaphragm pacemakers are traumatic, prone to complications such as iatrogenic infections and are relatively expensive, making them unsuitable for rehabilitation applications38. In contrast, the extracorporeal type stimulates the phrenic nerve motor points through the body surface, which allows the diaphragm to contract regularly without implantation. It is noninvasive and more convenient, and improves patient's tidal volume and diaphragm mobility while transforming diaphragm into muscle fibers with anti-fatigue function. This method is suitable for patients who are seriously ill and cannot participate in PR exercise training with a certain intensity.
Intensity
Many studies have shown that the intensity of exercise should follow the principle of individualized formulation. High-intensity exercise has greater physiological benefits for patients, and stable patients with good cardiopulmonary function and high compliance can be guided to carry out high-intensity exercise training39. Although there is a significant improvement in exercise capacity and physiological response after high-intensity exercise training, this method is not suitable for patients with severe disease and poor compliance. Therefore, intermittent exercise training with a gradual increase in exercise intensity can be used for patients with moderate to severe disease or higher40. The American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) recommends that Patients with COPD start with breathing muscle training, perform continuous exercises at a constant speed and low intensity, followed by overall endurance exercise. The absolute indicator of the upper limit of exercise is the presence of uncomfortable symptoms in patients, such as myocardial ischemia.
Frequency and duration
There is no clear standard for the duration of PR exercise training. Long-term exercise training has a certain effect on the improvement muscle strength therefore improving dyspnoea and making patients have a sensation of improved lung function. In general, the longer the duration of exercise training, the more significant the effect will be. The American Thoracic Society and the European Respiratory Society (ATS/ERS) believe that for Patients with COPD, it takes at least 8 weeks of training to bring about changes in the clinical indicators of patients and the indicators will plateau after training reaches 12 weeks. Some scholars41 have shown that 4 weeks of exercise training improved exercise capacity by 10% in patients with COPD that were over 50 years of age, while 5 weeks of intervention time was required to achieve the same results in patients over 60 years of age, suggesting that older patients need more exercise training time to get better PR effects. A study by Liang42 et al. showed that patients with COPD in stable phase undergo PR exercise training for 60 minutes per day and three times per week, continued to home rehabilitation after discharge will significantly improve the patients' pulmonary function. This is basically the same as the endurance exercise training program recommended by the AACVPR (20 to 60 minutes each time, 3 to 5 times a week).
Time
At present, in Australia and many other countries, PR programs tend to last 6-12 weeks with 2-3 supervised training sessions per week and last for about 60-90 minutes43. This is aligned with the latest ATS/ERS statement on PR which translates to 12-24 sessions (two training sessions per week) or 18-36 sessions (three training sessions per week)32. A 3-month outdoor Nordic walking exercise program for 60 elderly patients with moderate to severe COPD reported that 76% of participants achieved a minimum important difference (MID) increase in 6MWD after 20 supervised pulmonary rehabilitation training sessions, whereas only 20% of that group met the MID following 10 training sessions44.
Other Training Methods
Tai Chi
Tai Chi, which originated in China, is a systematic aerobic exercise training and is considered a suitable medium-intensity exercise training for patients with COPD. A Meta-study by Wu et al45, which included 824 patients with COPD, reported that compared with other exercise training, Tai Chi has a higher safety coefficient and for patients in stable phase, it can improve their dyspnea symptoms, increase exercise endurance and has a positive effect on BODE index, mental health status and quality of life. Chen et al46 suggested that Tai Chi can produce a stimulus similar to the effect of a treadmill on physiology of patients with COPD by exercising the muscles and joints of the whole body, making respiratory muscle fibers thicker, thus reducing respiratory rate and increasing the depth of effective breathing. Although there are many types of Tai Chi, there is no research on the most suitable type of taijiquan for patients with COPD. Future research should try to find the simplest and most effective types of Tai Chi.
Yoga
Yoga is an appropriate low-intensity exercise training for patients with COPD. Although there are no trials to prove the efficacy of flexibility training represented by yoga in chronic respiratory disease, it is commonly used in PR exercise training. Yoga stretches well the major muscle groups of patients, such as calves, quadriceps and biceps, and helps to increase the strength, flexibility, endurance and coordination of skeletal muscles. Also, pranayama (breathing techniques) in yoga enables patients to increase cardiopulmonary resistance through breath control, thus increasing lung capacity and decreasing respiratory rate. Studies47 have confirmed that yoga can improve the quality of life and exercise capacity of patients with COPD, and it may become an adjuvant therapy in PR exercise training in the future.
Conclusion
There are many methods of exercise assessment for patients with COPD and it is very crucial to select the most appropriate scales and tests to evaluate the effects of patients on their rehabilitation and prognosis. The following figure (figure 1) is a simple PR exercise training record sheet developed by us for patients with COPD. It records the results of pre- and post-exercise assessments in three dimensions: dyspnea, exercise capacity, and quality of life, as well as time, intensity, and frequency of exercise training. It is our goal to develop individualized exercise training prescriptions for patients with COPD. At present, more research is still needed to develop a systematic and standardized assessment method to provide a basis for the development of individualized exercise training programs for patients with COPD.
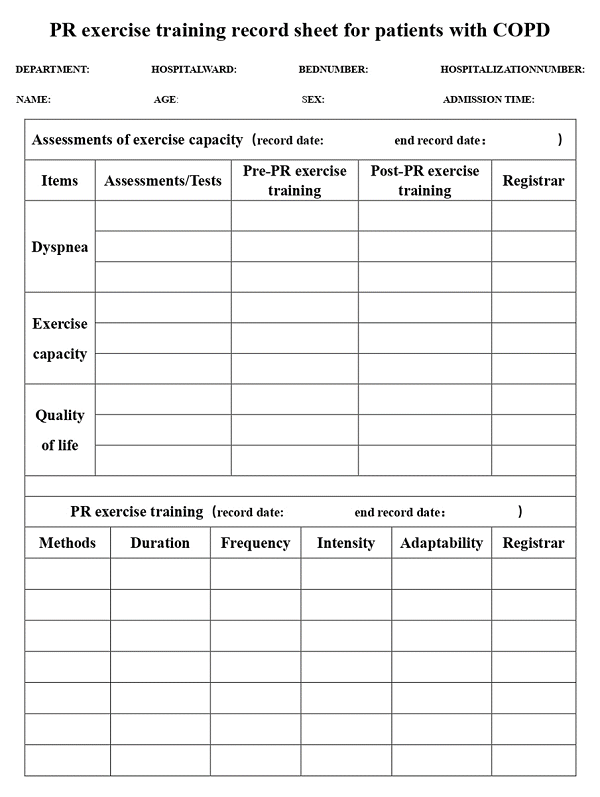
Figure 1: PR Exercise Training Record Sheet for Patients with COPD.
Conflict of Interest: The authors declare no conflict of interest.
Funding: This study received no special grant from any funding agency.
Acknowledgment: None
Author Contributions: The author contributions are as follow:
Li Chen, Conceptualization, Writing- Original draft preparation;
Jing Su, Writing- Reviewing and Editing.
References
- Ritchie AI, Wedzicha JA. Definition, Causes, Pathogenesis, and Consequences of Chronic Obstructive Pulmonary Disease Exacerbations. Clin Chest Med. 2020 Sep;41(3):421-438. doi: 10.1016/j.ccm.2020.06.007. PMID: 32800196; PMCID: PMC7423341.
- Montes de Oca M, Pérez-Padilla R. Global Initiative for Chronic Obstructive Lung Disease (GOLD)-2017: The alat perspective. Arch Bronconeumol. 2017 Mar;53(3):87-88. English, Spanish. doi: 10.1016/j.arbres.2017.01.002. Epub 2017 Feb 17. PMID: 28222935.
- Zhang XM, YangPY, Zhang YX, et al. Evidence summary of best practice literature for pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Journal of Nursing Science. 2020;35(12):94-98. doi: 10.3870/j.issn.1001-4152.2020.12.094
- Vonbank K, Strasser B, Mondrzyk J, et al. Strength training increases maximum working capacity in patients with COPD--randomized clinical trial comparing three training modalities. Respir Med. 2012 Apr;106(4):557-63. doi: 10.1016/j.rmed.2011.11.005. Epub 2011 Nov 26. PMID: 22119456.
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest. 2007 May;131(5 Suppl):4S-42S. doi: 10.1378/chest.06-2418. PMID: 17494825.
- Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004 Jun;23(6):932-46. doi: 10.1183/09031936.04.00014304. Erratum in: Eur Respir J. 2006 Jan;27(1):242. PMID: 15219010.
- Reddel HK, Taylor DR, Bateman ED, et al. American Thoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009 Jul 1;180(1):59-99. doi: 10.1164/rccm.200801-060ST. PMID: 19535666.
- Fabre C, Chehere B, Bart F, et al. Relationships between heart rate target determined in different exercise testing in COPD patients to prescribed with individualized exercise training. Int J Chron Obstruct Pulmon Dis. 2017 May 16;12:1483-1489. doi: 10.2147/COPD.S129889. PMID: 28553100; PMCID: PMC5439969.
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999 Jul;54(7):581-6. doi: 10.1136/thx.54.7.581. PMID: 10377201; PMCID: PMC1745516.
- Mador MJ, Rodis A, Magalang UJ. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest. 1995 Jun;107(6):1590-7. doi: 10.1378/chest.107.6.1590. PMID: 7781352.
- Bausewein C, Farquhar M, Booth S, et al. Measurement of breathlessness in advanced disease: a systematic review. Respir Med. 2007 Mar;101(3):399-410. doi: 10.1016/j.rmed.2006.07.003. Epub 2006 Aug 17. PMID: 16914301.
- Mahler DA, Weinberg DH, Wells CK, et al. The measurement of dyspnea. Contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984 Jun;85(6):751-8. doi: 10.1378/chest.85.6.751. PMID: 6723384.
- Ren L, Li QY. Evaluation of pulmonary rehabilitation and BODE index. Chinese Journal of Rehabilitation Medicine, 2009(08):763-765.
- Stringer W, Marciniuk D. The Role of Cardiopulmonary Exercise Testing (CPET) in Pulmonary Rehabilitation (PR) of Chronic Obstructive Pulmonary Disease (COPD) Patients. COPD. 2018 Dec;15(6):621-631. doi: 10.1080/15412555.2018.1550476. Epub 2018 Dec 30. PMID: 30595047.
- Erratum: ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2016 May 15;193(10):1185. doi: 10.1164/rccm.19310erratum. Erratum for: Am J Respir Crit Care Med. 2002 Jul 1;166(1):111-7. PMID: 27174486.
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014 Dec;44(6):1428-46. doi: 10.1183/09031936.00150314. Epub 2014 Oct 30. PMID: 25359355.
- Li N, Qiu C, Wei YL. Role of 6-minute walk test in chronic obstructive pulmonary diseases. Chinese Journal of Tissue Engineering Research, 2008, 12(011):2116-2119.
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014 Dec;44(6):1447-78. doi: 10.1183/09031936.00150414. Epub 2014 Oct 30. PMID: 25359356.
- Zainuldin R, Mackey MG, Alison JA. Prescription of walking exercise intensity from the incremental shuttle walk test in people with chronic obstructive pulmonary disease. Am J Phys Med Rehabil. 2012 Jul;91(7):592-600. doi: 10.1097/PHM.0b013e31824660bd. PMID: 22286894.
- Revill SM, Morgan MD, Singh SJ, et al. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax. 1999 Mar;54(3):213-22. doi: 10.1136/thx.54.3.213. PMID: 10325896; PMCID: PMC1745445.
- Larson JS. The MOS 36-item short form health survey. A conceptual analysis. Eval Health Prof. 1997 Mar;20(1):14-27. doi: 10.1177/016327879702000102. PMID: 10183310.
- Ge ZQ, Tian K, Zhao K. Analysis on the Improvement of Quality of Life in COPD Patients After Implementing Clinical Pathway Based on the EQ-5D. Chinese Hospital Management. 2016;36(04):35-37.
- Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis. 1992 Jun;145(6):1321-7. doi: 10.1164/ajrccm/145.6.1321. PMID: 1595997.
- Trappenburg JC, Touwen I, de Weert-van Oene GH, et al. Detecting exacerbations using the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2010 Sep 16;8:102. doi: 10.1186/1477-7525-8-102. PMID: 20846428; PMCID: PMC2949819.
- Huang TY, Moser DK, Hsieh YS, et al. Validation of Chinese version of the Modified Pulmonary Functional Status and Dyspnea Questionnaire with heart failure patients in Taiwan. Am J Crit Care. 2008 Sep;17(5):436-42. PMID: 18775999.
- Fan VS, Bridevaux PO, McDonell MB, et al. Regional variation in health status among chronic obstructive pulmonary disease patients. Respiration. 2011;81(1):9-17. doi: 10.1159/000320115. Epub 2010 Aug 17. PMID: 20720400.
- Karloh M, Fleig Mayer A, Maurici R, et al. The COPD Assessment Test: What Do We Know So Far?: A Systematic Review and Meta-Analysis About Clinical Outcomes Prediction and Classification of Patients Into GOLD Stages. Chest. 2016 Feb;149(2):413-425. doi: 10.1378/chest.15-1752. Epub 2016 Jan 12. PMID: 26513112.
- Rutten EP, Franssen FM, Engelen MP, et al. Greater whole-body myofibrillar protein breakdown in cachectic patients with chronic obstructive pulmonary disease. Am J Clin Nutr. 2006 Apr;83(4):829-34. doi: 10.1093/ajcn/83.4.829. PMID: 16600935.
- Burge AT, Cox NS, Abramson MJ, et al. Interventions for promoting physical activity in people with chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2020 Apr 16;4(4):CD012626. doi: 10.1002/14651858.CD012626.pub2. PMID: 32297320; PMCID: PMC7160071.
- Thompson PD, Arena R, Riebe D, et al. American College of Sports Medicine. ACSM's new preparticipation health screening recommendations from ACSM's guidelines for exercise testing and prescription, ninth edition. Curr Sports Med Rep. 2013 Jul-Aug;12(4):215-7. doi: 10.1249/JSR.0b013e31829a68cf. PMID: 23851406.
- Spruit MA, Singh SJ, Garvey C, et al. ATS/ERS Task Force on Pulmonary Rehabilitation. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013 Oct 15;188(8):e13-64. doi: 10.1164/rccm.201309-1634ST. Erratum in: Am J Respir Crit Care Med. 2014 Jun 15;189(12):1570. PMID: 24127811.
- Klionsky DJ, Abdel-Aziz AK, Abdelfatah S, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition). Autophagy. 2021 Jan;17(1):1-382. doi: 10.1080/15548627.2020.1797280. Epub 2021 Feb 8. PMID: 33634751.
- Joyner MJ, Casey DP. Regulation of increased blood flow (hyperemia) to muscles during exercise: a hierarchy of competing physiological needs. Physiol Rev. 2015;95(2):549-601. doi:10.1152/physrev.00035.2013
- Bickford LS, Hodgkin JE, McInturff SL. National pulmonary rehabilitation survey. Update. J Cardiopulm Rehabil. 1995 Nov-Dec;15(6):406-11. doi: 10.1097/00008483-199511000-00002. PMID: 8624965.
- Bjarnason-Wehrens B, Mayer-Berger W, Meister ER, et al. German Federation for Cardiovascular Prevention and Rehabilitation. Einsatz von Kraftausdauertraining und Muskelaufbautraining in der kardiologischen Rehabilitation. Empfehlungen der Deutschen Gesellschaft für Prävention und Rehabilitation von Herz-Kreislauferkrankungen e. V [The stakes of force perseverance training and muscle structure training in rehabilitation. Recommendations of the German Federation for Prevention and Rehabilitation of Heart-Circulatory Diseases e.v]. Z Kardiol. 2004 May;93(5):357-70. German. doi: 10.1007/s00392-004-0063-7. PMID: 15160271.
- Casaburi R, Porszasz J, Burns MR, et al. Physiologic benefits of exercise training in rehabilitation of patients with severe chronic obstructive pulmonary disease.[J]. Am J Respir Crit Care Med, 1997, 155(5):1541-1551.
- Levine S, Nguyen T, Kaiser LR, et al. Human diaphragm remodeling associated with chronic obstructive pulmonary disease: clinical implications. Am J Respir Crit Care Med. 2003 Sep 15;168(6):706-13. doi: 10.1164/rccm.200209-1070OC. Epub 2003 Jul 11. PMID: 12857719.
- Cooper CB. Exercise in chronic pulmonary disease: aerobic exercise prescription. Med Sci Sports Exerc. 2001 Jul;33(7 Suppl):S671-9. doi: 10.1097/00005768-200107001-00005. Erratum in: Med Sci Sports Exerc 2001 Sep;33(9):following table of contents. PMID: 11462076.
- Beauchamp MK, Nonoyama M, Goldstein RS, et al. Interval versus continuous training in individuals with chronic obstructive pulmonary disease--a systematic review. Thorax. 2010 Feb;65(2):157-64. doi: 10.1136/thx.2009.123000. Epub 2009 Dec 8. PMID: 19996334.
- Casaburi R, Patessio A, Ioli F, et al. Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis. 1991 Jan;143(1):9-18. doi: 10.1164/ajrccm/143.1.9. PMID: 1986689.
- Liang SY, Cen HH, Zheng ZG, et al. Compliance with pulmonary rehabilitation in patients with chronic obstructive pulmonary disease at different stages. The Journal of Practical Medicine. 2012;28(17):2966-2968. doi:10.3969/j.issn.1006-5725.2012.17.059.
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest 2007; 131(5 Suppl.): 4S–42.
- Breyer MK, Breyer-Kohansal R, Funk GC, et al. Nordic walking improves daily physical activities in COPD: a randomised controlled trial. Respir Res 2010;11:112.
- Wu W, Liu X, Wang L, et al. Effects of Tai Chi on exercise capacity and health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2014 Nov 7;9:1253-63. doi: 10.2147/COPD.S70862. PMID: 25404855; PMCID: PMC4230171.
- Chen YW, Hunt MA, Campbell KL, et al. The effect of Tai Chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses. Br J Sports Med. 2016 Apr;50(7):397-407. doi: 10.1136/bjsports-2014-094388. Epub 2015 Sep 17. PMID: 26383108.
- Yudhawati R, Rasjid Hs M. Effect of yoga on FEV1, 6-minute walk distance (6-MWD) and quality of life in patients with COPD group B. Adv Respir Med. 2019;87(5):261-268. doi: 10.5603/ARM.2019.0047. PMID: 31680225.
