Functional mobility in older practitioners of Liang Gong exercise
Felipe L. Belozo1, Naely Pivetta2, Victor A. R. Fernandes1,3, Rebeca S.M.N. Belozo1, Tatiane C. de Paula1, Carlos K. Katashima5, Andre K. Yamada4, Carlos Roberto Bueno Jr.4, Vagner R. R. Silva5*
1College of Physical Education - Network Faculty, Nova Odessa, SP, Brazil
2State University of Campinas (UNICAMP), Campinas, SP, Brazil
3Laboratory of Tissue Morphology. Jundiai Medical School. Jundiaí, SP, Brazil
4School of Physical Education and Sport of Ribeirao Preto, University of Sao Paulo, Ribeiro Preto, Brazil
5Postgraduate Program in Nutrition and Sport Sciences and Metabolism. School of Applied Sciences, University of Campinas (UNICAMP), Limeira, SP, Brazil
Abstract
Background: Falls can lead to several comorbidities and are considered a major cause of mortality in the elderly.
Objective: Herein, we evaluated functional mobility in older practitioners of Liang Gong exercise as a strategy to prevent falls.
Method: We evaluated 90 subjects (10 men and 80 women) using measures of body mass index (BMI), waist circumference (WC), abdominal circumference (AC), calf circumference (CC), 5 times sit to stand test (5TSS), and 4-meter gait speed test (4GST).
Results: Against our expectations, 68.88% of the participants presented low-performance in the 5TSS and 71.11% in the 4GST. In addition, we associated CC (considered a marker of sarcopenia) with the 5TSS using Pearson's correlation analysis but no statistical differences were found between the low-performance group and the high-performance group.
Conclusion: Our results showed that the majority of the older adults who have been practicing Liang Gong exercise for more than 6-months presented unsatisfactory results in the indices of functional mobility and we believe that a combination of resistance, functional and aerobics trainings would be more effective to improve it.
Introduction
Aging is a natural process characterized by a progressive loss of physiological functions such as hormonal and immune regulation, mobility and energetic metabolism. These physiological changes can lead to the development of obesity and sarcopenia and consequently, various chronic diseases such as cancer, diabetes, cardiovascular diseases, neurodegenerative diseases, and depression1. It is estimated that, by 2050, the world population aged over 60 will rise from 841 million to two billion, with approximately 434 million people been aged over 802,3.
According to the Physical Activity Guidelines Advisory Committee (PAGAC) the combination of physical exercises (aerobic, strength, balance, and flexibility) increases strength, gait speed and balance in daily activities of the elderly. On the other hand, the absence of physical exercise, or the poor manipulation of training variations, such as intensity and weekly frequency, may not present significant improvements in the functional and physical capacities of the elderly, thus being not able to decrease comorbidities and mortality resulting from falls4.
Falls are one of the main causes of morbidity, mortality, and health care costs in the elderly population5. It is reported that 28.7% of adults with 65 years or more fell in 2014 in the United States6. Between 2009 and 2015, the public hospital care system from Brazil spent around US$275 million on treatments and medical assistance of people over 60 years, which represented 39% of the total costs related to admission/hospitalizations. In this period, the elderly population in Brazil increased by 27% and, consequently, the intensive care costs increased 12%. In addition, the mortality increased from 9.8% to 11.2% and the greatest cause of hospitalization in the elderly population was falls7.
It is well known that physical activity can prevent or attenuate comorbidities and also prevent falls in the elderly population8-12. Despite advances in medicine aiming for a better aging process13-16, different non-pharmacological alternatives could be a great strategy to prevent or attenuate falls, reducing morbidity, mortality, and health care costs in elderly population.
Different studies have already described the effects of non-pharmacological therapeutic oriental practices to improve health in elderly populations, such as meditation17, Tai chi chuan18, Yoga19, apuncuture20 and Liang Gong exercises21. Recently, Liang Gong was described as a great strategy to improve health in subjects with dizziness21. Liang Gong is a Chinese therapeutic technique that uses firm and smooth movements with the objective of minimizing muscle tension, correct posture, optimize motor coordination, balance, and body awareness21. Once the benefits of Liang Gong are still poorly characterized, we evaluated if they could improve functional mobility in elderly practitioners. To measure the functional mobility in the elderly people, we applied two easy and low-cost functional evaluation tests, known as 5 Times Sit to Stand test (5TSS) and 4-meter gait speed test (4GST), both previously described in the literature22-29.
Methods
Study Population
The Ethical Committee of the University of Campinas approved the study protocols (CAAE: 95651918.2.0000.5404). This study is also registered in ClinicalTrials.gov (Register Number: RBR-6fgg7b) http://www.ensaiosclinicos.gov.br/rg/RBR-6fgg7b/. After providing the written informed consent, we recruited 106 elderly practitioners of Liang Gong (12 men and 94 women) from the “Centro de Melhor Idade” from Hortolândia city/Sao Paulo. The inclusion criteria were age over 60 years by 2019, be active and to practice Liang Gong activity at least two times a week, for more than 6 months. The Liang Gong exercise was offered by “Centro da Melhor Idade” in two classes on alternate days (40 minutes per class) and extra-activities such as embroidery, aquatic weight-bearing exercises, and adapted volleyball were offered to the subjects in other days. We considered as active only those participants who practice at least 150 minutes a week of physical activity4. A total of 90 individuals (10 men and 80 women) successfully completed all tests. 16 subjects were excluded based on severe medical conditions that could affect significantly their mobility or because the registration of data was incomplete (See Figure 1). In Tables 1 and 2 we present baseline and sociodemographic characteristics of participants.
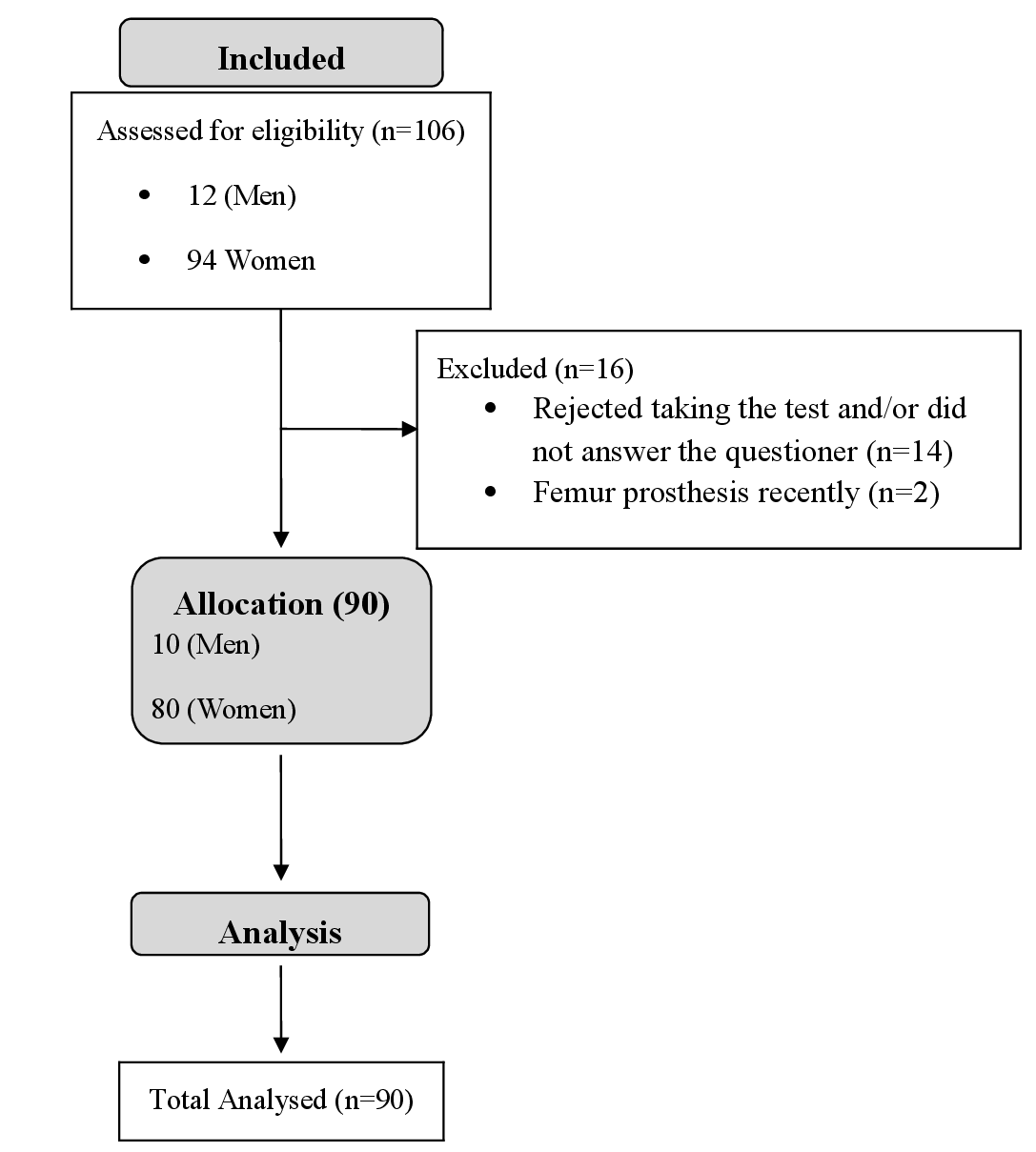
Figure 1. The flow of study subjects
Table 1. Characteristics of the subjects
|
|
MEN |
WOMEN |
|
|
N=10 |
N=80 |
|
Anthropomorphic data, mean |
|
|
|
Age (years) |
70,3±6.72 |
68,39±5.53 |
|
Heigh (cm) |
164,65±9.63 |
153,41±5.77 |
|
Weight (kg) |
74,66±14.35 |
68,67±12.84 |
|
BMI (Body weight index) |
27,4±4.17 |
29,16±5.20 |
|
Abd. circunference (cm) |
99,51±9.59 |
96,08±10.37 |
|
Waist (cm) |
93,91±7.92 |
86,92±13.12 |
|
Hips (cm) |
98,8±5.59 |
102,76±10.63 |
|
WHR (Waist/Hips ratio) |
0,95±0.05 |
0,84±0.10 |
|
Right calf (cm) |
35,11±3.43 |
|
|
Left calf (cm) |
34,96±3.06 |
|
|
Risk regarding abd. circunference, No (%) |
|
|
|
Normal |
3 (30) |
5 (6) |
|
Increased |
4 (40) |
11 (14) |
|
Substantially increased |
3 (30) |
64 (80) |
Table 2. Sociodemographic and clinical characteristics of the participants
|
|
MEN |
WOMEN |
|
|
N=10 |
N=80 |
|
Declared ethnicity, No (%) |
|
|
|
White |
6 (60) |
42 (53) |
|
Pards |
4 (40) |
32 (40) |
|
Black |
0 (0) |
6 (7) |
|
Education, No (%) |
|
|
|
Illiterate |
2 (20) |
12 (15) |
|
0-4 years (Fundamental I) |
4 (40) |
33 (41) |
|
5-9 years (Fundamental II) |
3 (30) |
23 (29) |
|
> 9 years (High School) |
1 (10) |
9 (11) |
|
> 12 years (Graduated) |
0 (0) |
1 (1) |
|
> 16 years (Pos-graduated) |
0 (0) |
2 (3) |
|
Marietal Status, No (%) |
|
|
|
Married |
8 (80) |
28 (35) |
|
Single |
1 (10) |
12 (15) |
|
Divorced |
0 (0) |
5 (6) |
|
Widow(er) |
1 (10) |
33 (41) |
|
No answer |
0 (0) |
2 (3) |
|
Health condition, No (%) |
|
|
|
Fall in the last 12 months |
2 (20) |
22 (28) |
|
Difficulty climbing stairs |
3 (30) |
17 (21) |
|
Hypertension |
7 (70) |
41 (51) |
|
Diabetes |
1 (10) |
24 (30) |
|
Arthritis |
2 (20) |
9 (11) |
|
Arthrosis |
5 (50) |
26 (33) |
|
Osteoporosis |
1 (10) |
10 (13) |
|
Osteopenia |
0 (0) |
2 (2) |
|
Other diseases |
- |
3a, 2b,1c,1d,1e, 1f (11) |
|
a: Thyroid dysfunction |
|
|
|
b: Labyrinthitis |
|
|
|
c: Cardiac Arrhythmia |
|
|
|
d: Dyslipidaemia |
|
|
|
e: Asthma |
|
|
|
f: Fibromyalgia |
|
|
Anthropometrics data
The subjects were classified into underweight, normal weight, overweight, or obese according to the body mass index (BMI). The BMI was calculated using the mathematical formula kg/m2 with the cut-off point provided by the World Health Organization (WHO) (BMI > 30 kg/m2)30. Body weight (kilograms) was verified using a commercial digital scale (100g) and height (in meters) using a measuring tape (precision of 01mm).
The waist circumference (WC) was measured and classified according to31, with the subject in the anatomical position and feet slightly apart. The evaluator stood in front of the participant and measured WC with a tape measure at the smallest perimeter of the abdomen. Three measurements were performed and the mean was used for the analysis.
Abdominal circumference (cm) (AC) was collected and classified according to31, with the participant in the anatomical position, feet slightly apart. The evaluator performed the measurement at the height of the navel with a measuring tape. Three measurements were performed and the mean was used for the analysis.
Calf circumference (cm) (CC) was measured with the subjects in an anatomical position with the feet slightly apart, distributing body weight evenly between the lower limbs. The evaluator faced the participant, and performed the measurement with the measuring tape at the point of greatest circumference of the right or left calf. The classification was made according to the literature32,33. Three measurements were performed and the mean was used for the analysis.
Tests
5 Times Sit to Stand test (5TSS): This test was performed using a chair with a backrest and no arms, and a seat height of 43 cm. Timer, paper and pen were used to record the time (in seconds). The chair was positioned against the wall for greater stability. After being given explanations about how to perform the test, the participants were allowed to have a time of familiarization. The test began with the subject in a standing position. At the evaluator’s command “attention, now”, the participant performed five movements of sitting and standing up, fully touching the buttocks on the seat of the chair and performing a complete extension of the knees at the end of the movement. The chronometer was stopped when the subject had completed the movement five times, finishing in the initial position. Two measurements were recorded and the best time was adopted as the final result. The final results were classified as low-performance according to age cut-offs as follows; 61 to 69 (>11.4 seconds), 70 to 79 (>12.6 seconds), and 80 to 89 (>14.8 seconds). Below this time, the subject was classified as high-performance, according to the literature22-24.
4-meter gait speed test (4GST): This test was performed on the volleyball court, with a non-slip floor to avoid accidents. The initial and final points were measured with metric tape and signalized with coloured masking tape. In order to prevent deceleration of participants before four meters, the floor was signalized at 4 meters and 4.5 meters and the participants were instructed to walk along the distance to the second lane (4.5 meters) in normal rhythm25 but the chronometer was stopped when the subject reached the 4 meters lane. After explaining the details of the test we gave time to participants to familiarize themselves with the test. All participants started in the rest position and standing. The evaluator started the chronometer after the command “attention, now” and finished when the participant crossed the line of 4 meters with both feet. Two measurements were performed and the best time was taken as the final result. The speed was calculated according to the time (in seconds) divided by 4 (meters). The final results were classified as low-performance (≥0.8 meter/second) and high-performance (≤0.8 meter/second) according to the literature25.
Sociodemographic analyses
Sociodemographic analyses, including ethnicity, educational level, marital status and health conditions were obtained using a questionnaire at the screening interview.
Statistical Analysis
Statistical analyses were performed using GraphPad Prism version. 8.2.1. A two-tailed Pearson's correlation was used for the correlation analyses, and the Mann Whitney test, when necessary. Differences were considered when P-value < .05. Data were expressed as mean ± standard error of the mean (SEM).
Results
Initially, we recruited 106 physically active elder subjects for this study (12 men and 94 women); however, 16 subjects were excluded, resulting in a final of 90 participants (10 men and 80 women). Figure 1 presents the flowchart of the participants. Table 1 presents the characteristics of the participants and table 2, the sociodemographic and clinical characteristics.
Herein we measured the levels of functional mobility22-29 of 90 physically active elderly subjects in an indirect manner using the 5TSS and 4GST. We classified the test results into low-performance and high-performance, according to the literature22-25. Our results showed that 68.88% of the participants presented low-performance in the 5SST and 71.11% low-performance in the 4GST (Figure 2A and B).
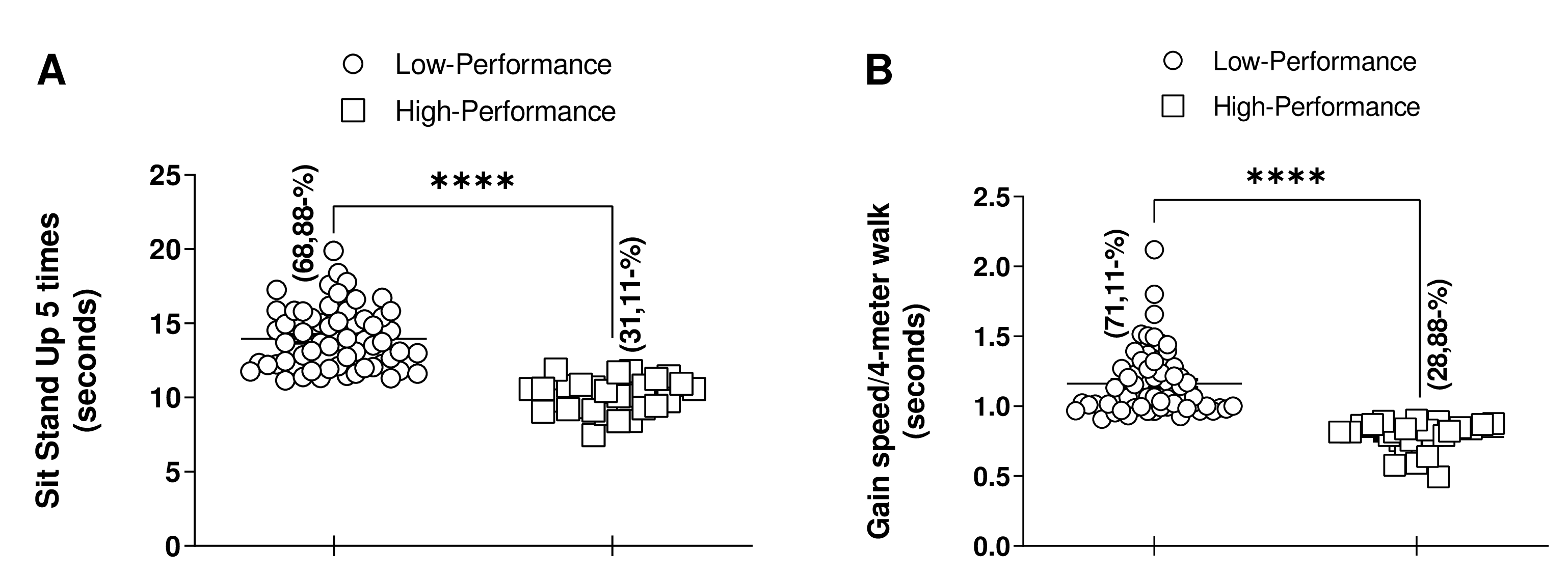
Figure 2. Analysis of 5 times sit to stand test or the 4-meter gait speed test. (A) Analyses of 5 times sit to stand test (n=62 low-performance and n=28 high-performance); (B) Analyses of 4-meter gait speed test (n=64 low-performance group and n=26 high-performance group); The percentage (%) analyses were calculated from the multiplication of the total subjects in the low-performance group or high-performance group by 100 and then divided by the total number of participants. ****p < 0.0001. Mann Whitney test, (*p < 0.05).
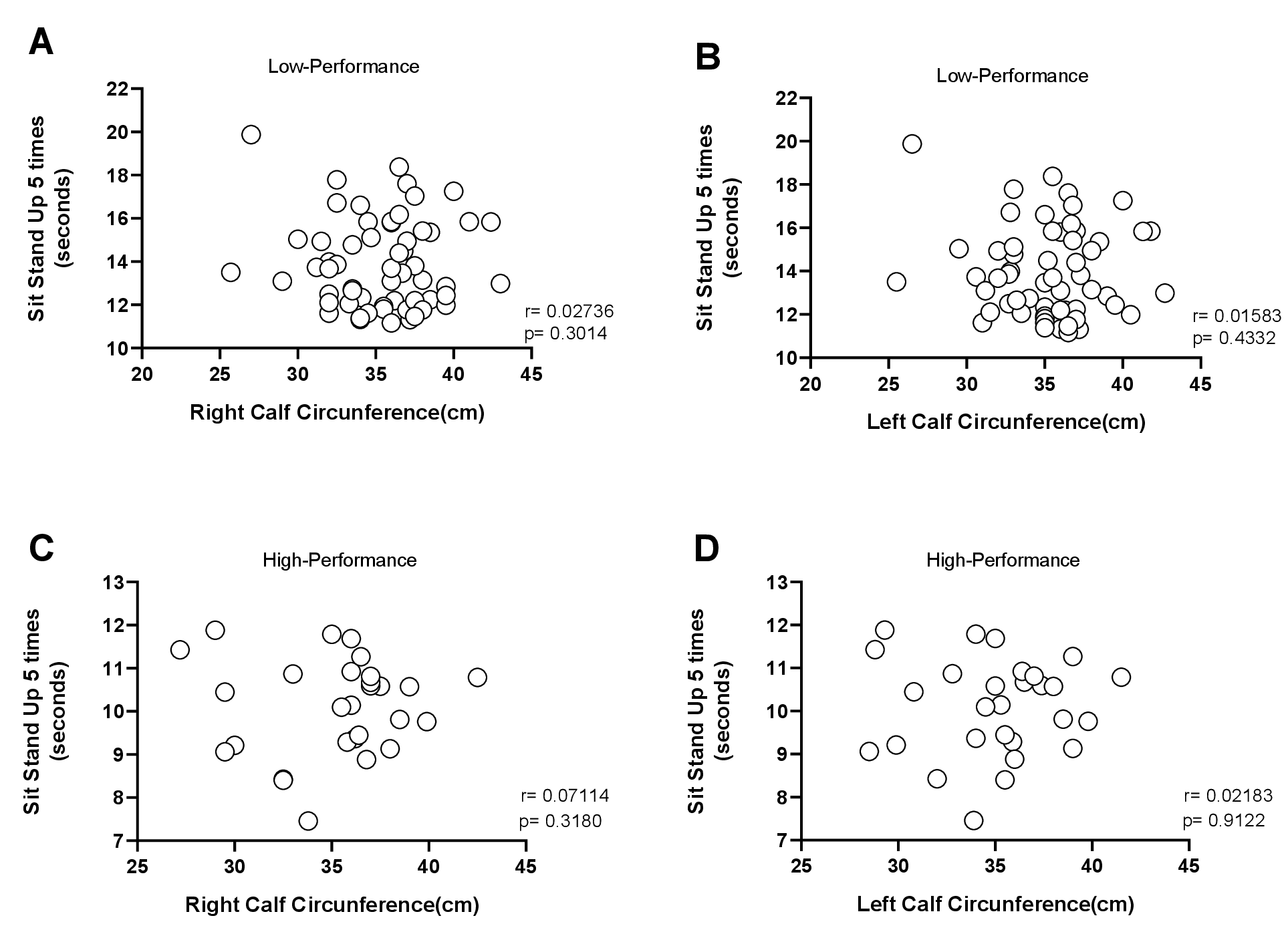
Figure 3. Pearson's correlation analysis between 5 times sit to stand test with calf circumference. (A and B) Right or left calf circumference of low-performance group (n=62); (C and D) Right or left calf circumference of high-performance group (n=28). two-tailed Pearson's correlation was used for the correlation analyses (*p < 0.05).
According to the European Working Group on Sarcopenia in Older People (EWGSOP), the reduction in physical performance is a marker used to indirectly measure sarcopenia34. Previously studies suggest that calf circumference (above 31cm) indicates preserved muscle mass and could be a marker associated with sarcopenia32,33. Since most of our participants presented reduced physical performance (Figure 2A and B), we postulated that our group of participants could be sarcopenic; therefore, we measured calf circumference. The mean calf circumference was 35.17±3.45 for the right calf and 35.08±3.33 for the left calf (Table 1). These results indicate that the group studied is not sarcopenic, according to the literature32,33. Using correlation analysis, we associated the calf circumference with the 5TSS but our results demonstrated no correlations between calf circumference and the 5TSS in either group (low and high-performance groups) (Fig. 3A-D). Thus, we concluded that calf circumference measurement does not represent an adequate strategy to evaluate physical performance, since our group presented a circumference above that recommended (> 31cm) but the majority of participants showed low performance in the tests.
Discussion
It is estimated that the world population aged over 60 years will increase over the next decades2,3. Consequently, the number of aging-related diseases will increase6,7,35. Reduction in functional mobility in the lower and upper limbs in the older population is one of the main reported causes of decreased self-confidence in balance and consequently a major factor of falls35. Currently, it is proposed that falls are the main cause of morbidities, mortality, and health care costs in elderly people6,7,35. Thus, strategies to prevent or attenuate falls are important for health care system. The current study aimed to evaluate the functional mobility in older practitioners of Liang Gong exercise.
Physical activity can help to improve health. In this line, therapeutic oriental medicine has been proven to be efficient in improving the quality of life of older populations17-21. However, we observed that, according to functional mobility tests, the elderly participants of Liang Gong exercises presented poor mobility. The results showed that 68.88% of the participants presented low-performance in the 5TSS and 71.11% in the 4GST, both markers of functional mobility22-25. Liang Gong is a Chinese therapeutic technique and although the movements cover the whole body21, this activity does not have characteristics of resistance training and functional movements. In addition, it is important to highlight that the volume and intensity of the Liang Gong exercises could not have been enough to increase the functional mobility. Our participants have been practicing Liang Gong two times a week on alternate days (40 minutes per class). Thus, we cannot discard the possibility that with an increase in the volume and intensity of this type of exercise we would have achieved better results. Therefore, studies with clinical trials are necessary to better understand the effects of the volume and intensity of the Liang Gong session in elderly population.
Since the natural aging process leads to the atrophy of type II fibers, indispensable for strength36, the resistance training should be included in activity programs for older populations, in order to prevent reduction in muscle strength35,37,38. It was already demonstrated that well elaborated and well prescribed resistance training programs improve muscle strength and physical performance in older populations, even in those individuals diagnosed with sarcopenia9,39,40.
The most common method of practicing resistance training is using equipment; however, for some elder people, the use of equipment may be difficulty for several reasons, including disability and poor strength. Therefore, training with body weight can be a good strategy in those cases, improving strength, increasing muscle mass and reducing body fat41,42. Corroborating these findings, a recent study showed that resistance training without equipment improved muscle strength and functional fitness in healthy older subjects. The authors noticed that eccentric resistance training was more effective than concentric training for improving lower limb strength, mobility, and postural stability in older adults43. However, other types of training programs are important to maintain health in older people17-21,39. In our opinion, Liang Gong exercises could be more effective if combined with resistance training sessions; once recent findings suggest that the optimum training should contain multicomponent exercises, including both aerobic and resistance exercises39,44.
As mentioned in the methodology session, the “Centro de Melhor Idade” offered extra-activities to the participants of Liang Gong exercises, such as aquatic weight-bearing exercises. If well oriented and practiced with quality, this extra activity could improve muscle strength. Balsamo et al.45, reported that both resistance training and aquatic weight-bearing exercises can prevent loss of bone mineral density in postmenopausal women over fifty years of age when compared to the respective control group. In our study, most of the participants practiced aquatic weight-bearing exercises, but, unfortunately, as a recreational activity, without periodization and overload, and, consequently, without intention to gain muscle strength. Thus, we hypothesized that the association of Liang Gong exercises with aquatic weight-bearing using periodization protocols could be an alternative to improve muscle strength in older populations.
Another relevant finding in our study is regarding the evaluation of sarcopenia. Some studies characterize sarcopenia when the calf circumference is less than 31cm32,33 and a correlation between sarcopenia and reduction in physical performance was already reported12,34. Thus, we were curious to compare these two parameters, once the average of calf circumference in our study group was 35 cm (see table 1). Interestingly, our results do not agree with the literature. When we performed the 5TSS and 4GST, most of the subjects presented low-performance (see figure 2A and B) within the established time, based on age22-25. This led us to conclude that calf circumference is not the better way to evaluate sarcopenia related to physical performance. Despite being one of several markers of sarcopenia, its evaluation in an isolated manner seems to be inconclusive. Similar results were previously observed in a large group of community-dwelling elderly females46. Taken together, we did not see strong positive effects of the Liang Gong exercises in the functional mobility of elderly people, but we believe that if associated with others activities in a multicomponent program of exercises, including aerobic and anaerobic training, the practice of Liang Gong may improve the quality of life of this population.
Conclusion
Our results showed that the majority of the older Liang Gong exercise practitioners who have been performing this activity for more than 6-months presented unsatisfactory results regarding functional mobility. To reach better functional mobility, the literature recommends the combination of resistance, functional and aerobics trainings. Multicomponent exercises seem to improve the daily functional movements such as walking, sitting and standing and consequently, being able to increase the independence of the individual and to decrease the risk of falls.
Study limitations
In our study, we presented the effects of Liang Gong on physical function in an indirect manner and we failed to perform pre- and post-test comparison. We were not able to control extra activities that were performed by the individuals. Additionally, we had proportionally more accession of women than men in the study, which reflects the greatest concern with health between women, but may have led to a sex difference in physical performance between the genders.
Acknowledgements
The authors would like to thank the “Centro de Melhor Idade” of Hortolândia/ /SP for enabling us to evaluate the participants, Dr. Alfredo Wagner da Conceicao for technical collaboration in the study, and Dr. Thais Fenz Araujo for intellectual and technical support.
Declaration of Conflicting Interests
No potential conflicts of interest are declared by the authors of this study.
Funding
The author(s) received no financial support for this study.
References
- Lopez-Otin C, Blasco MA, Partridge L, et al. The hallmarks of aging. Cell. 2013;153:1194-1217. doi:10.1016/j.cell.2013.05.039.
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2015 - Highlights (ST/ESA/SER.A/368).
(2015). - Sanderson WC, Scherbov S, Gerland P. Probabilistic population aging. PLoS One. 2017;12:e0179171. doi:10.1371/journal.pone.0179171.
- Dipietro L, Campbell WW, Buchner DM, et al. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med Sci Sports Exerc. 2019;51:1303-1313. doi:10.1249/mss.0000000000001942.
- Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet. 2013;381:752-762. doi:10.1016/s0140-6736(12)62167-9.
- Hartholt KA, Lee R, Burns ER, et al. Mortality From Falls Among US Adults Aged 75 Years or Older, 2000-2016. JAMA. 2019;321:2131-2133. doi:10.1001/jama.2019.4185.
- Dias RD, Barros JV. Burden of hospitalisation among older people in the Brazilian public health system: a big data analysis from 2009 to 2015. J Epidemiol Community Health. 2019;73:537-543. doi:10.1136/jech-2018-210783.
- Sherrington C, Fairhall N, Wallbank G, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic Review. Br J Sports Med. 2019. doi:10.1136/bjsports-2019-101512.
- de Mello RGB, Dalla Corte RR, Gioscia J, et al. Effects of Physical Exercise Programs on Sarcopenia Management, Dynapenia, and Physical Performance in the Elderly: A Systematic Review of Randomized Clinical Trials. J Aging Res. 2019;2019:1959486. doi:10.1155/2019/1959486.
- Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25 Suppl 3:1-72. doi:10.1111/sms.12581.
- Yamada M, Kimura Y, Ishiyama D, et al. Synergistic effect of bodyweight resistance exercise and protein supplementation on skeletal muscle in sarcopenic or dynapenic older adults. Geriatr Gerontol Int. 2019;19:429-437. doi:10.1111/ggi.13643.
- Distefano G, Standley RA, Zhang X, et al. Physical activity unveils the relationship between mitochondrial energetics, muscle quality, and physical function in older adults. J Cachexia Sarcopenia Muscle. 2018;9:279-294. doi:10.1002/jcsm.12272.
- Lamming DW, Ye L, Sabatini DM, et al. Rapalogs and mTOR inhibitors as anti-aging therapeutics. J Clin Invest. 2013;123:980-989. doi:10.1172/jci64099.
- Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell. 2014;159:709-713. doi:10.1016/j.cell.2014.10.039.
- Madeo F, Eisenberg T, Pietrocola F, et al. Spermidine in health and disease. Science. 2018;359. doi:10.1126/science.aan2788.
- Longo VD, Antebi A, Bartke A, et al. Interventions to Slow Aging in Humans: Are We Ready? Aging Cell. 2015;14:497-510. doi:10.1111/acel.12338.
- Chetelat G, Lutz A, Arenaza-Urquijo E, et al. Why could meditation practice help promote mental health and well-being in aging? Alzheimers Res Ther. 2018;10:57. doi:10.1186/s13195-018-0388-5.
- Tao J, Liu J, Liu W, et al. Tai Chi Chuan and Baduanjin Increase Grey Matter Volume in Older Adults: A Brain Imaging Study. J Alzheimers Dis. 2017;60:389-400. doi:10.3233/jad-170477.
- Youkhana S, Dean CM, Wolff M, et al. Yoga-based exercise improves balance and mobility in people aged 60 and over: a systematic review and meta-analysis. Age Ageing. 2016;45:21-29. doi:10.1093/ageing/afv175.
- Yu SW, Lin SH, Tsai CC, et al. Acupuncture Effect and Mechanism for Treating Pain in Patients With Parkinson's Disease. Front Neurol. 2019;10:1114. doi:10.3389/fneur.2019.01114.
- Lopes AL, Lemos SMA, Figueiredo PHS, et al. Impact of lian gong on the quality of life of individuals with dizziness in primary care. Rev Saude Publica. 2019;53:73. doi:10.11606/s1518-8787.2019053001234.
- Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64-68. doi:10.1519/00139143-200608000-00004.
- Alexandre TS, Meira DM, Rico NC, et al. Accuracy of Timed Up and Go Test for screening risk of falls among community-dwelling elderly. Rev Bras Fisioter. 2012;16:381-388. doi:10.1590/s1413-35552012005000041.
- Buatois S, Miljkovic D, Manckoundia P, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56:1575-1577. doi:10.1111/j.1532-5415.2008.01777.x.
- Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881-889. doi:10.1007/s12603-009-0246-z.
- Melo TAd, Duarte ACM, Bezerra TS, et al. The Five Times Sit-to-Stand Test: safety and reliability with older intensive care unit patients at discharge. Rev Bras Ter Intensiva. 2019;31:27-33. doi:10.5935/0103-507X.20190006.
- Bohannon RW, Bubela DJ, Magasi SR, et al. Sit-to-stand test: Performance and determinants across the age-span. Isokinet Exerc Sci. 2010;18:235-240. doi:10.3233/IES-2010-0389.
- Lord SR, Murray SM, Chapman K, et al. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. The journals of gerontology. Series A, Biological sciences and medical sciences. 2002;57:M539-M543. doi:10.1093/gerona/57.8.m539.
- Buatois S, Perret-Guillaume C, Gueguen R, et al. A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys Ther. 2010;90:550-560. doi:10.2522/ptj.20090158.
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894, i-xii, 1-253 2000.
- Maximo RO, Santos JLF, Perracini MR, et al. Abdominal obesity, dynapenia and dynapenic-abdominal obesity as factors associated with falls. Braz J Phys Ther. 2019;23:497-505. doi:10.1016/j.bjpt.2018.10.009.
- Rolland Y, Czerwinski S, Abellan Van Kan G, et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008;12:433-450. doi:10.1007/bf02982704.
- Rolland Y, Lauwers-Cances V, Cournot M, et al. Sarcopenia, calf circumference, and physical function of elderly women: a cross-sectional study. J Am Geriatr Soc. 2003;51:1120-1124. doi:10.1046/j.1532-5415.2003.51362.x.
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412-423. doi:10.1093/ageing/afq034.
- Hopewell S, Copsey B, Nicolson P, et al. Multifactorial interventions for preventing falls in older people living in the community: a systematic review and meta-analysis of 41 trials and almost 20 000 participants. Br J Sports Med. 2019. doi:10.1136/bjsports-2019-100732.
- Wilkinson DJ, Piasecki M, Atherton PJ. The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res Rev. 2018;47:123-132. doi:10.1016/j.arr.2018.07.005.
- Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA. 2019;321:2092-2100. doi:10.1001/jama.2019.5795.
- Tessier AJ, Wing SS, Rahme E, et al. Physical function-derived cut-points for the diagnosis of sarcopenia and dynapenia from the Canadian longitudinal study on aging. J Cachexia Sarcopenia Muscle. 2019;10:985-999. doi:10.1002/jcsm.12462.
- Pedersen BK. Which type of exercise keeps you young? Curr Opin Clin Nutr Metab Care. 2019;22:167-173. doi:10.1097/mco.0000000000000546.
- Fisher JP, Steele J, Gentil P, et al. A minimal dose approach to resistance training for the older adult; the prophylactic for aging. Exp Gerontol. 2017;99:80-86. doi:10.1016/j.exger.2017.09.012.
- Tsuzuku S, Kajioka T, Sakakibara H, et al. Slow movement resistance training using body weight improves muscle mass in the elderly: A randomized controlled trial. Scand J Med Sci Sports. 2018;28:1339-1344. doi:10.1111/sms.13039.
- Watanabe Y, Tanimoto M, Oba N, et al. Effect of resistance training using bodyweight in the elderly: Comparison of resistance exercise movement between slow and normal speed movement. Geriatr Gerontol Int. 2015;15:1270-1277. doi:10.1111/ggi.12427.
- Katsura Y, Takeda N, Hara T, et al. Comparison between eccentric and concentric resistance exercise training without equipment for changes in muscle strength and functional fitness of older adults. Eur J Appl Physiol. 2019;119:1581-1590. doi:10.1007/s00421-019-04147-0.
- Northey JM, Cherbuin N, Pumpa KL, et al. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med. 2018;52:154-160. doi:10.1136/bjsports-2016-096587.
- Balsamo S, da Mota LMH, de Santana FS, et al. Resistance training versus weight-bearing aquatic exercise: a cross-sectional analysis of bone mineral density in postmenopausal women. Rev Bras Reumatol. 2013;53:193-198.
- Kusaka S, Takahashi T, Hiyama Y, et al. Large calf circumference indicates non-sarcopenia despite body mass. J Phys Ther Sci. 2017;29:1925-1928. doi:10.1589/jpts.29.1925.
