Effects of Whole-Body Vibration on Fibromyalgia: Is There Any Evidence to Support Clinical Practice?
Jousielle Márcia dos Santos1, Vanessa Amaral Mendonça1,2,3, Vanessa Gonçalves Cesar Ribeiro3, Vinicius Cunha Oliveira2, Sueli Ferreira da Fonseca3, Hércules Ribeiro Leite1,2,3, Ana Carolina Coelho de Oliveira1, Pedro Henrique Scheidt Figueiredo1,2,3, Mario Bernardo-Filho4, Vanessa Pereira Lima1,2, Ana Cristina Rodrigues Lacerda1,2,3*
1Postgraduate Program in Rehabilitation and Functional Performance, Universidade Federal dos Vales do Jequitinhonha e Mucuri (UFVJM), Diamantina, Minas Gerais, Brazil
2Physiotherapy Department, Universidade Federal dos Vales do Jequitinhonha e Mucuri (UFVJM), Diamantina, Minas Gerias, Brazil
3Multicenter Postgraduate Program in Physiological Sciences, Sociedade Brasileira de Fisiologia (SBFis), Diamantina, Brazil
4Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, Brazil
Abstract
Introduction: Whole Body Vibration (WBV) exercise has been widely applied in the clinical practice. Thus, the present review aims to provide an updated review of current literature on the effects and efficacy of WBV alone or combined with exercise in patients with fibromyalgia (FM).
Methods: The works were identified and selected from the PubMed, Cochrane-Central-Register-of-Controlled-Trials and Physiotherapy Evidence-Database (PEDro) databases. Randomized controlled trials (RCTs) and case-control studies were selected without language restrictions. Articles including single or multiple WBV sessions have been identified.
Results: Nine works were included in the review (1 case-control study and 8 RCTs). The average PEDRro score was 7.44 ± 0.95. The sample size varied from 20 to 46 participants, involving only women diagnosed with FM. The outcomes identified were pain, balance, quality of life, fatigue and disability. Only one study investigated FM-related inflammatory biomarkers.
Conclusions: Although WBV treatment appears to be safe and feasible, there is limited evidence to support WBV application in clinical practice in patients with FM.
Introduction
Fibromyalgia (FM) is a chronic disorder whose etiology remains unknown. FM is characterized by generalized inflammatory pain, tenderness that persists for at least three months and the presence of at least 11 of the 18 specified tender points. The FM prevalence in the general population is approximately 2-3%, where 90% are women1.
FM is associated with several deficiencies and activity limitations, including fatigue, disrupted sleep, impaired cognition, poor functional capacity, headaches, arthritis, muscle spasm, tingling and balance dysfunctions2. FM is also related to other diseases, such as rheumatoid arthritis and ankylosing spondylitis3-5. Thus, several approaches have been used to minimize deficiencies and limitations of activity and increase the quality of life of this population, including pharmacological and non-pharmacological therapies6-9.
There is strong evidence showing that both pharmacological and non-pharmacological approaches can be effective6,10-12. Non-pharmacological therapies include physical interventions such a yoga, Tai chi, walking, and whole-body vibration (WBV) exercise6,13,14. During WBV, the individual is positioned on the platform and stimuli are transmitted to the body, where the intensity is determined by peak-to-peak displacement, amplitude, frequency and acceleration of the oscillation15-17. Authors speculate that WBV therapy can improve balance, pain, and fatigue; however, the results are contradictory18-20.
There have been three reviews examining the effects of WBV stimulus on symptoms associated with FM6,21,22. However, these reviews have examined only articles published between 2008 and 2015. Other articles have been published more recently23,24. There is limited evidence on the efficacy or effectiveness of this approach in the FM population because of the limited methodological quality of the previous studies. In addition, we report the importance of describing work that address the International Classification of Functioning and Disability and Health (ICF).
The importance of addressing ICF in recent studies refers to the fact that this classification can provide unified and standardized language as well as a framework for describing health and health-related states. The most important feature of CIF is the possibility of measuring the impact of the disease on the individual and the environment, making it a useful tool for research approaches. Considering that the instrument covers the patient as a whole, it is able to analyze the individual for functionality and the sociocultural condition in which it is inserted.
Therefore, in an attempt to address these gaps, the purpose of the present systematic review was to provide an updated analysis of the research on the effects and efficacy of WBV alone or combined with exercise. Studies that indirectly addressed the (ICF), as well as biological parameters related to inflammatory profile related to FM, are contextualized.
Methods
Electronic database searches and selection strategy
A search was conducted on the Cochrane Library, the Physiotherapy Evidence Database (PEDro) and the PubMed database up to May 2018. Keywords used in our search strategy were “fibromyalgia” and “vibration”. These activities were supervised by experts in the field of WBV in FM. We used P.I.C.O. components (Patients/Population, Intervention, Comparison, Results) to stablish elements to our search strategy, where people with FM (P); WBV Therapy (I); Comparison between WBV versus minimal intervention and additional (C); outcomes of interest were body functions and structures, activities and participation (O). Duplicate articles were manually removed by one of the authors.
We inserted a flow chart delineating the complete selection process in the systematic review (Figure 1). In our study, the inclusion and exclusion criteria for the studies were described as follows. Inclusion criteria: studies examining adults with fibromyalgia; including single or multiple WBV sessions that used the PICO approach (Patients, Intervention, Control, Results, and Study Design). Exclusion criteria: PEDro score <5. The search was completed on the 26th of May 2018, with no submission deadline being imposed, the selection was performed by two independent evaluators.
Types of participants
We included works that examined adults with ï¬bromyalgia in the review. We selected works that used published criteria for diagnosis (or classiï¬cation) of ï¬bromyalgia. Until recently, the American College of Rheumatology (ACR) 1990 criteria served as the standard for classifying individuals as having ï¬bromyalgia25 when they have experienced widespread pain lasting longer than three months and when pain can be elicited at 11 of 18 speciï¬c tender points on the body with 4 kg tactile pressure. A newer preliminary diagnostic tool — ACR 2010 (1) — does not rely upon an examination of a physical tender point and is available as both a clinician-administered tool and a survey questionnaire26. This measure includes a Widespread Pain Index (19 areas representing anterior and posterior axes and limbs) in addition to a Symptom Severity Scale containing items related to secondary symptoms such as fatigue, sleep disturbance, cognition, and somatic complaints. Scores on both measures are used to determine whether a person qualiï¬es as meeting a “case deï¬nition” of ï¬bromyalgia. This tool has been used to classify 88.1% of cases that meet ACR 1990 criteria, and it permits ongoing monitoring of symptom change in people with a current or previous diagnosis of ï¬bromyalgia1. Although measurements focusing on tender point counts have been widely applied in clinical and research settings, methods described by Wolfe 2010 and Wolfe 2011 promise to classify people with ï¬bromyalgia more efï¬ciently, while allowing improved monitoring of disease status over time. Although differences among published ï¬bromyalgia diagnostic/classiï¬cation criteria are known, we considered all published criteria to be acceptable and comparable for the purposes of this review.
Types of interventions
We examined trials that studied WBV exercise interventions (e.g., moving or holding a standing position while on an oscillating platform) regardless of the frequency, duration, or intensity of exercise sessions. We have provided an example of a WBV exercise intervention in Appendix 2. We categorized interventions by the duration of the program (e.g., “short” < seven weeks; “intermediate” seven to 12 weeks, “long” > 12 weeks) and by frequency of training per week (e.g., once per week, twice per week, and three or more times per week). Comparative interventions included control (e.g., placebo or sham intervention).
Assessing the risk of bias
The PEDro scale was used to assess the risk of bias in the selected articles. This is a scale that classifies the methodological quality of work evaluating physiotherapeutic interventions. The PEDro scale was chosen because of its special design and ability to provide an overview of the external and internal validity of the studies. The assessment of the methodological quality of the studies was performed independently by two investigators. A third investigator was contacted in case of disagreement, and the assessment was resolved by consensus. Studies that already provided a PEDro score were re-evaluated by one of the researchers. (Note: there was total agreement between PEDro and researcher scores). Table 1 shows the consensus results for each article.
Determining the level of evidence
The level of evidence was determined using the PEDro Scale guidelines, a scale that classifies the methodological quality of studies evaluating physiotherapeutic interventions.
Data extraction
Data were extracted from the selected articles by one of the authors. This extraction was checked by a second author. Any disagreement was discussed and ultimately resolved by a third author if the contact with the original author of the article could not be established.
For each selected article, the following data were extracted: (a) the sample and protocol characteristics, namely, the sample size, age, and activity of the control and WBV groups (Table2), and (b) the vibration therapy details, namely, the type of device and its oscillation (acceleration, frequency, peak-to-peak displacement and amplitude), the duration of the intervention, the number of WBV sessions, the number of vibration series, the rest period, and the exposure duration in each series (Table3).
Synthesis and Data Analysis
A descriptive analysis of measurements of WBV effects was performed on each selected result. In the articles with significant results, we calculated the changes between the groups using the SES (Standard Effect Size) values, which were analyzed through means and standard deviations. The effect size was considered to be small (for SES values = 0.2), medium (SES = 0.5) and large (SES = 0.8) in accordance with the definitions of Cohen (1992)27.
Results
Article selection
A total of 40 articles were ideintified in the electronic search of the Cochrane (12 articles), PubMed (15 articles) and PEDro (13 articles) databases. After checking duplicates, fifteen articles were removed, and remained twenty-five articles that were checked (title and abstract). After screening, reimaning ten articles that were evaluated about eligibility. Thereafter, one article was excluded becauso scored lower than 5 in Pedro Scale. Finally, nine articles were included in our systematic review, with two different study designs (eg, randomized case or control) and two types of intervention (eg single session or multiple sessions). (Figure 1).
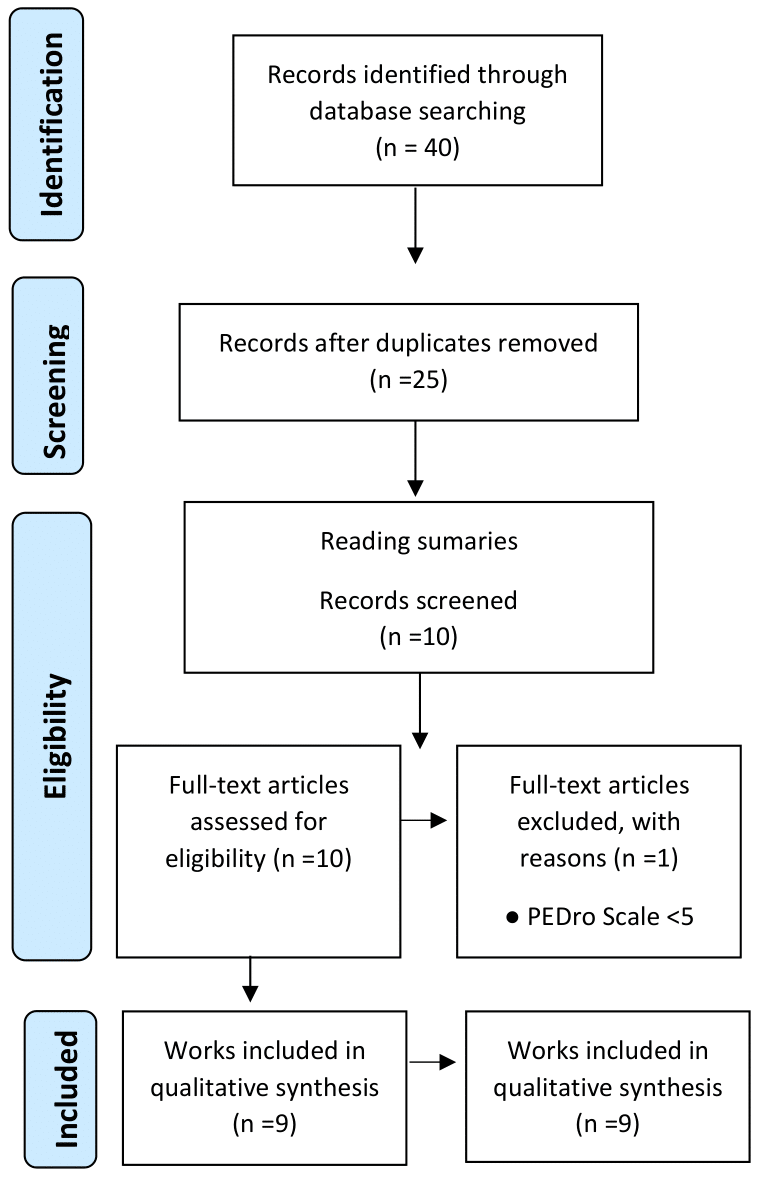
Figure 1: Flow chart
Risk of bias
According to the PEDro scale score, the score of the studies ranged from 5 to 8 points. The average (SD) score was 7.44 ± 0.95. The lowest scores were obtained for questions three (“concealed allocation”), five (“there was blinding of all subjects”), six (“there was blinding of all therapists”; this result reflects the fact that it is difficult to blind a WBV therapist), and seven (“assessor-blinded”). Good scores were obtained for questions one (“eligibility criteria were specified”), four (“the groups were similar at baseline”), eight (“measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups”), nine (“the results of between-group statistical comparisons are reported for at least one key outcome”), and eleven (“the study provides both point measures and measures of variability for at least one key outcome”) (Table 1).
Table 1. Risk of bias and level of evidence.
|
Criterion |
Study |
||||||||
|
Comparison (9 works) |
|||||||||
|
Works with PEDro score≥6. PEDro score was obtained by checking the items on the Physiotherapy Evidence Database site. |
|||||||||
|
Ribeiro et al 201823 |
Alev et al 201724 |
Sanudo et al 201328
|
Adsuar et al 201229
|
Sanudo et al 201230
|
Olivares et al 201132
|
Sanudo et al 201031
|
Gusi et al 201033
|
Alentorn et al 200834
|
|
|
Eligibility criteria |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Random Allocation |
|
X |
X |
X |
X |
X |
X |
X |
X |
|
Concealed Allocation |
|
|
X |
|
X |
X |
|
X |
|
|
Baseline comparability |
|
X |
X |
X |
X |
X |
X |
X |
X |
|
Patient Blinded |
|
|
|
|
|
|
|
|
|
|
Therapist Blinded |
X |
|
|
|
|
|
|
|
|
|
Assessor Blinded |
X |
X |
|
X |
|
X |
X |
X |
X |
|
Adequate follow-up (>85%) |
X |
|
X |
X |
X |
X |
X |
X |
X |
|
Intention to treat analysis |
|
|
X |
|
|
X |
|
X |
|
|
Between-group-comparisions |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Poin estimates and variability |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Total PEDro score |
5 |
5 |
7 |
6 |
6 |
8 |
6 |
8 |
6 |
|
Sample size ≥ 50 |
N |
N |
N |
N |
N |
N |
N |
N |
N |
Risk of bias and level of evidence. Distribution Points Scale PEDro: N: criterion not completed; X: criterion filled.
Study Characteristics
The characteristics of the studies using the PICO (Patients, Intervention, Control, Outcomes, and Study design) approach are summarized in Table 2. All nine studies were performed with adult and older women with FM, and the sample size varied from 20 to 46 participants.
WBV parameters
WBV equipment
One study used the Power Plate vibratory platform23, seven studies used the Galileo vibratory platform24,28-33 and one study used the FitVibe platform34. The Galileo vibratory platform produces side-alternating stimulus, whereas the FitVibe and Power Plate platforms produce a synchronous vibration.
Frequency and amplitude
Studies differed in terms of amplitude and frequency of vibration. Seven studies used lateral alternating path stimulus vibration employing an amplitude of 2-4 mm and a frequency of 12.5 - 30 Hz, and two studies used vertical synchronous stimulus vibration employing an amplitude of 2-4 mm and a frequency of 30-40 Hz. (Table 3).
Performance on the platform
The postures used in the studies also varied. In five studies, subjects maintained a dynamic stance on the platform during vibration23,28,29,32,33, whereas subjects of three studies maintained a static posture on the platform during vibration24,30,31, and the subjects maintained static and dynamic postures during vibration in only one study34. All the works specified that both feet were always flat on the platform during vibration. The knee angle varied between 45o and 130o in the static model and between 90o and 180o in the dynamic model (Table 3).
Table 3. Details of vibratory therapy
|
Vibration Therapy Details
|
||||||||
|
Study |
WBV type and comercial name |
Type treatment |
Frequency Amplitude Acceleration |
Series duration |
Rest |
Posture |
Comparison protocol |
Additional treatment |
|
Ribeiro et al 201823 |
FitVibe
Synchronous
|
Session single |
40 Hz 4mm 25.7 g |
8x40 seconds |
30 seg |
Dynamic squattin |
None |
None |
|
Alev et al 201724 |
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 4 weeks (4x weeks) |
30 Hz 2 mm 7.2
|
1x 5 minute |
0 |
Dynamic squattin |
Yes |
None |
|
Sanudo et al 201328
|
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 6 weeks (2x weeks) |
30 Hz 4 mm 14.5 g |
6x30 seconds |
45 seconds |
Dynamic squattin |
Yes |
Yes |
|
Adsuar et al 201229
|
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 12 weeks (3x weeks) |
30 Hz 4 mm 14.5 |
30 seconds (4 weeks) 45 seconds (8 weeks) 60 seconds (12 weeks) |
60 seconds |
Dynamic squattin |
Yes |
None |
|
Sanudo et al 201230
|
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 6 weeks (2x weeks) |
20 Hz 3 mm 4.8 g |
3x45 seconds (bilateral) 2x 15 seconds (unilateral) |
120 seconds |
Static unilateral and dynamic bilateral squattin |
Yes |
None |
|
Olivares et al 201132
|
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 12 weeks (3x weeks) |
30 Hz 4 mm 14.5 g |
30 seconds (4 weeks) 45 seconds (8 weeks) 60 seconds (12 weeks) |
30 seconds |
Dynamic squattin |
Yes |
None |
|
Sañudo et al 201031
|
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 6 weeks (2x weeks) |
20 Hz 3 mm 4.8 g |
3x 45 seconds (bilateral) 2x 15 seconds (unilateral) |
120 seconds |
Static unilateral and dynamic bilateral squattin |
Yes |
None |
|
Gusi et al 201033 |
Galileo Fitness Vibration
Side-alternating way |
Session Multiple 12 weeks (3x weeks) |
12.5 Hz 4mm 2.5 g |
30 seconds (4 weeks) 45 seconds (8 weeks) 60 seconds (12 weeks) |
30 seconds |
Dynamic squattin |
Yes |
None |
|
Alentorn et al 200834
|
Power Plate Synchronous
|
Session Multiple 6 weeks (2x weeks) |
30 Hz 2 mm 7.2 g |
6x30 seconds |
180 seconds |
Dynamic squattin |
Yes |
Yes |
Details of vibratory therapy including acceleration: frequency and amplitude of oscillation, duration of intervention, number of WBV sessions and number of vibration series, rest period and duration of exposure in each series.
Key measurements and effects
The outcomes with the highest level of completion and considered to represent the outcomes were pain, balance, quality of life, fatigue and disability24,28-34. Only one study analyzed biological aspects related to FM that characterize modeling of the inflammatory profile23 (Table 2).
Table 2. Studies characteristics.
|
Study, Type of study and Recruitment |
Participants Characteristics |
Inclusion criterion |
Exclusion criterion |
Findings |
Conclusion |
||||
|
Sample size and groups |
Age (years) |
Exercise type |
|||||||
|
Ribeiro et al 201823 Prospective paired case control Brazilian Journal of Medical and Biological Research |
40 participants (20 WBV 20 Control) |
WBV 52.16±1.81 CT 51.05±1.90 |
Dynamic squatting |
Women diagnosed with FM according to the ACR. |
Any concomitant disease that could be exacerbated by physical activity, pregnancy, inflammatory diseases and degenerative, joint, respiratory or cardiovascular diseases. |
Modulation of the inflammatory profile in women with FM. |
A single acute short and short WBV session might improve the inflammatory state in FM patients, reaching values close to those of healthy mates in their baseline state. |
||
Avel et al2017 (2)RCT24Complement Ther Clin Pract |
20 participants FM (10 WBV 10 Control)
|
WBV 56.2 ± 3.2 CT 58.1 ± 2.3 |
|
Diagnosis of FM, based on criteria the ACR. |
One or more possible contraindications for a WBV intervention (acute hernia, thrombosis, diabetes, epilepsy, metabolic or neuromuscular diseases, osteoporosis, osteoarthritis, orthopedic injuries and prostheses). |
Significant improvement of the EX + VCI group in the QIF questionnaire. |
The WBV was effective in reducing the symptoms of fibromyalgia. |
||
|
Sanudo et al 2013 (3) RCT28 J Rehabil Med
|
46 participants FM ÷3 Gr. Ex.(15) Ex+VCI.(15) Control(16) |
WBV 57.15±6.80 CT 55.5 ± 7.9 EX+ 62.28 ±9.8
|
static squatting |
Women diagnosed with FM according to the ACR. |
Contraindications for a WBV intervention (acute hernia, thrombosis, diabetes, epilepsy, metabolic or neuromuscular diseases, osteoporosis, osteoarthritis, orthopedic injuries and prostheses), use of drugs that could interfere in the control of balance, were also omitted. |
Traditional exercises associated with VCI improves balance in FM. |
Traditional exercise program, supplemented with full-body vibratory training, improved balance in women with fibromyalgia. This might be a key factor in the prevention of falls in patient with FM. |
||
|
Adsuar et al 2012 (4)29 RCT
|
41 participants (20 WBV 21 Control) |
WBV 53.0±12.0 CT 52.4±10.8
|
Dynamic squatting |
FM had been diagnosed by a rheumatologist in accordance with the diagnostic criteria of the ACR. |
History of severe trauma, frequent migraines, peripheral nerve entrapment, inflammatory rheumatic diseases, severe psychiatric illness, disease that prevents physical loading, pregnancy, participation in a psychological or physical therapy program, or participation in regular physical exercise more than once a week for 30 min or longer over a 2-week period in the last 5 years. |
Statically, there was an improvement in the balance of 57.1% in general stability and 66.6% in anteroposterior stability. |
Whole-body vibration therapy effectively improves the static balance in patients with FM. |
||
|
Sañudo et al 2012 (5) RCT30 |
30 participants (15 WBV 15 Control) |
WBV 55.0±12.1 CT 53.4±8.8 |
static squatting |
Diagnosis of FM, based on criteria the ACR. |
Disease possible contraindications for a WBV intervention (acute hernia, thrombosis, diabetes, epilepsy, metabolic or neuromuscular diseases, osteoporosis, osteoarthritis, orthopedic injuries and prostheses). |
Significant differences were found (p <0.05) between the study groups for the Mid-Lateral Stability Index (MLSI). |
Women with FM can increase their MLSI by participating in a traditional 6-week exercise program with supplemental WBV. This fact can have implications for the prevention of falls in this group of patients. |
||
|
Olivares et al 2011 (6)32 RCT |
36 participants (18 WBV 18 Control) |
WBV 53.0±12.0 CT 54.4 ±10.8
|
Dynamic squatting |
The assignment ofa diagnosis of FM by a rheumatologist in accordance with the diagnostic criteria of the ACR.
|
The following exclusion criteria were applied: a history of severe physical trauma inï¬ammatory rheumatic disease, severe psychiatric illness, any comorbid disease that imight prevent physical loading, pregnancy, participation in another psychologic or physical therapy program, or a history of regular physical exercise during the previous 5 years. |
Significant differences were found in the QIF scores compared to the CT group. |
WBV was a viable intervention that provided improvement in QoL in women previously not physically trained with FM. |
||
|
Sanudo et al 2010 (7)31 RCT
|
30 participants (15 WBV 15 Control) |
WBV 57.89±6.23 CT 60.13±9.42
|
Dynamic squatting and static |
Diagnosed with FM based on the ACR.
|
Exclusion criteria included the presence of inï¬ammatory rheumatic disorders or degenerative joint diseases, psychiatric disorders, and respiratory or cardiovascular diseases that could interfere with the physical activity programme. Subjects who were performing structured physical activity for at least two days a week or had psychological therapy during the six months prior the study were also excluded |
Significant improvements in all measured outcomes were found from the start in both groups. However, it was accompanied by reductions in the SF36 scores of 9.8% in the CT group. |
Women with FMS can gain additional health benefits by participating in a traditional 6-week exercise program with supplemental IVC. |
||
|
Gusi et al 2010 (8)33 RCT |
41 participants (21 WBV 20 Control) |
WBV 53.0±12.0 CT 52.4±10.8 |
Dynamic squatting |
Women Diagnosed by a rheumatologist in accordance with the diagnostic criteria of the ACR.
|
Exclusion criteria included history of severe trauma, frequent migraines, peripheral nerve entrapment, inï¬ammatory rheumatic diseases, severe psychiatric illness, other diseases that prevent physical loading, pregnancy, participation in another psychological or physical therapy program, or participation in regular physical exercise more than once a week for 30 minutes during any 2-week period in the last 5 years. |
Based on the ITT analysis, the dynamic balance of the vibration group improved by 36% compared to the baseline, whereas the control group remained unchanged. The differences in the dynamic equilibrium index were predicted (61%, P <0.001). |
The vibration program was useful and feasible to improve the dynamic balance in women with FM. These new results support new research aimed at the development of physiotherapy programs using controlled vibration. |
||
|
Alentorn et al 2008 (9)34
|
36 participants (12 WBV 12 WBV+EX 11 Control) |
WBV 55.2±3.4 CT 53.7 ± 2.7 EX 59.3 ±2.3 |
Dynamic squatting and static |
Diagnosis of FM, according to the ACR.
|
Limitation, cardiovascular, pulmonary, or metabolic disease that would preclude exercise, or when participating in any other study (Fig. 1). Written informed consent was obtained from each subject prior to participation in the study according to procedures approved by the Committee on Biomedical Ethics of the Jordi Gol Gurina Foundation (Spain). |
Significant improvements in pain parameters in the VCI + EX group compared to CT group. |
The results suggest that a traditional 6-week exercise program with supplemental IVC safely reduces pain and fatigue, while exercise alone does not induce improvement. |
||
Studies characteristics using the PICO (Patients, Intervention, Control, Outcomes, and Study design) approach. ACR: American College of Rheumatology.
Pain
Pain is the most important symptom in FM, but it was specifically assessed in only one study, which reported improvement in pain (Effect Size f = 0.74), as compared to basal and control groups34. However, pain is part of the Fibromyalgia Impact Questionnaire (FIQ) used to evaluate quality of life in FM.
Balance
Four studies28-30,33 evaluated the effects of WBV therapy on balance, specifically dynamic and static balance. One study showed that WBV significantly improved the dynamic balance (Effect Size f = 0.46) in the WBV group33. In three studies, mediolateral and anteroposterior indices were both measured (Effect Size f = 0.60; Effect Size f = 0.66). Only the mediolateral stability index improved in two studies29,30, and no statistical differences were observed in the third study30.
Quality of life
Only one study evaluated the health-related quality of life using the health status questionnaire (SF-36), which evaluates limitations, body pain, vitality, mental health and general health perception. This study showed WBV training improved SF-36 scores (Effect Size f = 0.42)31.
Fatigue and disability
Three studies evaluated the effect of WBV therapy on fatigue and disability24,32,34. They used the QIF questionnaire that measures physical function (activities of daily living), and general work. Improvements in fatigue (Effect Size f = 0.48) and disability (Effect Size f = 0.60 - Effect Size f = 0.62) domains by WBV were observed.
Effects of a single WBV session
Ribeiro et al. 201823 (40 participants) investigated the acute effects of a single WBV session on biomarkers of inflammation in FM and healthy-paired subjects, demonstrating an improvement in inflammatory profile with only one vibration session. Thus, subjects with FM reached values close to those of healthy individuals with paired anthropometric characteristics. The mechanism of neuroendocrinology appeared to be exercise-induced modulation towards a greater adaptation to the stress response in these patients.
Effects of multiple WBV sessions
Eight studies (320 participants) investigated the effects of multiple WBV sessions. The training period was approximately 4-12 weeks. Significant results were related to the improvement of dynamic balance28,33, static balance29,30,33, reduction of pain, improvement of disability and quality of life through QIF24,32,34 and improvement in muscle strength, functional performance and fatigue31.
ICF Approaches
Five of the nine studies assessed outcomes related to structure and function domains, i.e., balance tests, six-minute walk test, strength and fatigue28-31,33, three of the nine studies addressed the results related to participation, i.e., quality of life (SF-36, and FIQ)24,31,32, one study evaluated depression through the Beck Depression Index questionnaire, related to environmental and personal aspects24.
Discussion
This review evaluated the possible benefits of WBV in women with FM. Nine studies analyzed and presented an adequate methodological basis with a risk of bias evaluated by the PEDro scale (> 6), totalizing 320 participants. Of these, 300 obtained a confirmed diagnosis of FM by the Rheumatologist, which can guarantee greater reliability in the results. There was a heterogeneity of results, participants and intervention protocols that made a meta-analysis impossible. The results of this review have demonstrated that WBV therapy can improve various FM symptoms, for example, inflammatory parameters, disability, pain, quality of life, poor balance and platform fatigue23,24,28-34.
The duration of treatment might be extremely relevant in assessing the effects of WBV on FM fatigue. Five studies involved only 4-6 weeks of complementary vibration therapy24,28,30,31,34, and one study involved 12 weeks of vibratory therapy32. This last study reported a significant improvement in fatigue compared to the control group, whereas the other five studies did not show significant improvements among the groups. Thus, we suppose that the effect of WBV therapy on fatigue is the result of adaptations to multiple sessions. Moreover, a rigorous and methodical analysis of which protocol would be appropriate for the objective of the study seems necessary because the type of protocol used and the exercise modality could influence the evaluation of the effects of WBV on some symptoms of FM35.
We emphasize the importance of the standardization of the terminology in WBV studies because each study addresses different concepts and terms (e.g., platform type, synchronous-asynchronous-alternating), which makes the interpretation and replication of used protocols difficult17,36.
Regarding the result for balance, there were differences between the studies. These discrepancies might reflect differences between WBV protocols or different vibrating platform stimuli (Galileo and Power Plate). Thus, there is a need for even more clarified protocols to avoid the occurrence of discrepancies in the results. The most commonly used exercise for WBV in patients with FM was the exercise of dynamic or static squatting. It has not yet been investigated whether one modality of squatting is superior to another. Some WBVT devices also feature vibratory handles or straps that are attached to the platform so that isometric exercises for the upper extremities can be performed. Whether these vibration training applications for the upper body are useful or effective in patients with FM has yet to be investigated.
Only one study investigated the effect of a single WBV session on inflammatory parameters in FM. Although this study has shown that this stimulus seems to improve the inflammatory state in patients with FM, reaching values close to those found in paired patients in the basal state, a gap remains with respect to the possible physiological adaptations. We emphasize the importance of further studies on this subject that can contribute to understanding the etiology of FM. A correlation of FM with a neuroendocrine and inflammatory profile has been observed37.
Many patients may report difficulties in performing daily tasks, and it is necessary to approach the context of ICF, which helps to understand and shift the axis of the disease to the health axis. This new approach might allow the evaluation of the complete experience of the individual, investigating the contextual factors (personal and environmental) that can lead to limitations in activity and participation. Although the studies reviewed herein were not directed by the ICF, many of the variables evaluated could have been analyzed in the context of ICF. Thus, we suggest that further studies be performed considering at least one outcome in each ICF domain.
Although important findings are described, this review presents some limitations because of the (i) small number of studies using WBV in FM; (ii) wide variation in the vibration protocol and (iii) evaluation of different outcomes; (iv) as expected for studies with this intervention, blinded patients are not possible. The literature search was performed in three electronic databases: the Cochrane Library, the Physiotherapy Evidence Database (PEDro) and PubMed, and, therefore, some studies might not have been identified by the research. We updated the survey periodically.
Conclusion
WBV can be an alternative therapy for FM patients, modulating the inflammatory profile, improving the balance, disability, quality of life, fatigue and pain of this population. However, the small number of studies using WBV on FM and its wide variation in protocol of vibration, intervention and measurements are insufficient to substantiate treatment strategies and approaches. In general, authors become optimistic about the effects of WBV for individuals with FM, stating that research suggests that patients with FM can significantly improve if they participate in a personalized treatment. Nevertheless, there is limited evidence to support WBV in FM patients.
References
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. The american college of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research. 2010; 62: 600-10.
- Boomershine CS. A comprehensive evaluation of standardized assessment tools in the diagnosis of fibromyalgia and in the assessment of fibromyalgia severity. Pain Research and Treatment. 2012; 2012.
- Buskila D, Neumann L. Fibromyalgia syndrome (fm) and nonarticular tenderness in relatives of patients with fm. The Journal of rheumatology. 1997; 24: 941-4.
- Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: Report of the multicenter criteria committee. Arthritis Rheum. 1990; 33: 160–172.
- Fan A, Pereira B, Tournadre A, et al. editors. Frequency of concomitant fibromyalgia in rheumatic diseases: Monocentric study of 691 patients. Seminars in arthritis and rheumatism; 2017. Elsevier.
- Bidonde J, Busch AJ, van der Spuy I, et al. Whole-body vibration exercise training for fibromyalgia. The Cochrane Library 2017; 26:917-55.
- Tomas-Carus P, HÄkkinen A, Gusi N, et al. Aquatic training and detraining on fitness and quality of life in fibromyalgia. Medicine & Science in Sports & Exercise. 2007; 39: 1044-50.
- Verstappen FT, van Santen-Hoeuftt HMS, Bolwijn PH, et al. Effects of a group activity program for fibromyalgia patients on physical fitness and well-being. Journal of Musculoskeletal Pain. 1997; 5: 17-28.
- Arnold C, Faulkner R, Gyurcsik N. The relationship between falls efficacy and improvement in fall risk factors following an exercise plus educational intervention for older adults with hip osteoarthritis. Physiotherapy Canada. 2011; 63: 410-20.
- Wang C, Schmid CH, Fielding RA, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: Comparative effectiveness randomized controlled trial. Bmj. 2018; 360: k851.
- Redondo JR, Justo CM, Moraleda FV, et al. Longâterm efficacy of therapy in patients with fibromyalgia: A physical exerciseâbased program and a cognitive-behavioral approach. Arthritis Care & Research. 2004; 51: 184-92.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. Jama. 2004; 292: 2388-95.
- Busch AJ, Webber SC, Brachaniec M, et al. Exercise therapy for fibromyalgia. Current pain and headache reports. 2011; 15: 358.
- Worrel LM, Krahn LE, Sletten CD, et al. Treating fibromyalgia with a brief interdisciplinary program: Initial outcomes and predictors of response. Mayo Clinic Proceedings 2001. Elsevier.
- Martín J, Torre F, Padierna A, et al. Impact of interdisciplinary treatment on physical and psychosocial parameters in patients with fibromyalgia: Results of a randomised trial. International journal of clinical practice. 2014; 68: 618-27.
- Rauch F, Sievanen H, Boonen S, et al. Reporting whole-body vibration intervention studies: Recommendations of the international society of musculoskeletal and neuronal interactions. Journal of musculoskeletal & neuronal interactions. 2010; 10.
- Cardinale M, Lim J. Electromyography activity of vastus lateralis muscle during whole-body vibrations of different frequencies. The Journal of Strength & Conditioning Research. 2003; 17: 621-4.
- Baniak LM, Pierce CS, Hiester E, et al. Calf muscle pump stimulation as a means to reduce symptoms of fibromyalgia syndrome. Biological research for nursing. 2015; 17: 334-9.
- Bennett RM editor. Emerging concepts in the neurobiology of chronic pain: Evidence of abnormal sensory processing in fibromyalgia. Mayo Clinic Proceedings 1999. Elsevier.
- Valencia M, Alonso B, Alvarez M, et al. Effects of 2 physiotherapy programs on pain perception, muscular flexibility, and illness impact in women with fibromyalgia: A pilot study. Journal of manipulative and physiological therapeutics. 2009; 32: 84-92.
- Moretti E, Tenório A, Holanda L, et al. Efficacy of the whole-body vibration for pain, fatigue and quality of life in women with fibromyalgia: A systematic review. Disability and rehabilitation. 2018; 40: 988-96.
- Collado-Mateo D, Adsuar JC, Olivares PR, et al. Effects of whole-body vibration therapy in patients with fibromyalgia: A systematic literature review. Evidence-Based Complementary and Alternative Medicine. 2015; 2015: 719-82.
- Ribeiro V, Mendonça V, Souza A, et al. Inflammatory biomarkers responses after acute whole body vibration in fibromyalgia. Brazilian Journal of Medical and Biological Research. 2018; 51: 1414-431.
- Alev A, Mihriban A, Bilge E, et al. Effects of whole body vibration therapy in pain, function and depression of the patients with fibromyalgia. Complementary therapies in clinical practice. 2017; 28: 200-3.
- Wolfe F, Smythe HA, Yunus MB, et al. The american college of rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum.1990;33:160-72.
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: A modification of the acr preliminary diagnostic criteria for fibromyalgia. Journal of rheumatology 2011;38:1113-22.
- Cohen J. A power primer. Psychological Bulletin. 1992; 112: 155–159.
- Sañudo Corrales FdB, Carrasco L, Hoyo Lora Md, et al. Changes in body balance and functional performance following whole-body vibration training in patients withfibromyalgia syndrome: A randomized controlled trial. Journal of rehabilitation medicine. 2013; 678-84.
- Adsuar J, Del Pozo-Cruz B, Parraca J, et al. The single-leg stance static balance in women with fibromyalgia: A randomized controlled trial. The Journal of sports medicine and physical fitness. 2012; 52: 85-91.
- Sañudo B, de Hoyo M, Carrasco L, et al. Effect of whole-body vibration exercise on balance in women with fibromyalgia syndrome: A randomized controlled trial. The Journal of Alternative and Complementary Medicine. 2012; 18: 158-64.
- Sañudo B, Galiano D, Carrasco L, et al. Aerobic exercise versus combined exercise therapy in women with fibromyalgia syndrome: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2010; 91: 1838-43.
- Olivares PR, Gusi N, Parraca JA, et al. Tilting whole body vibration improves quality of life in women with fibromyalgia: A randomized controlled trial. The Journal of Alternative and Complementary Medicine. 2011; 17: 723-8.
- Gusi N, Parraca JA, Olivares PR, et al. Tilt vibratory exercise and the dynamic balance in fibromyalgia: A randomized controlled trial. Arthritis Care & Research. 2010; 62: 1072-8.
- Alentorn-Geli E, Padilla J, Moras G, et al. Six weeks of whole-body vibration exercise improves pain and fatigue in women with fibromyalgia. The Journal of Alternative and Complementary Medicine. 2008; 14: 975-81.
- Rittweger J, Ehrig J, Just K, et al. Oxygen uptake in whole-body vibration exercise: Influence of vibration frequency, amplitude, and external load. International journal of sports medicine. 2002; 23: 428-32.
- Cochrane D, Stannard S. Acute whole body vibration training increases vertical jump and flexibility performance in elite female field hockey players. British journal of sports medicine. 2005; 39: 860-5.
- Bordoni B, Marelli F, Morabito B, et al. Fascial preadipocytes Another missing piece of the puzzle to understand fibromyalgia? Open access rheumatology research and reviews. 2018; 10: 27.
